We are breaking down the basics of diastolic dysfunction into easy to understand blogs! Last week we discussed the topic of diastole and the 4 stages that occur during this phase within the cardiac cycle. If you missed it, you can read it here! This week, we are going to go a step further and discuss the physiology in regards to the 4 stages of diastole. We are going to cover:
The term physiology refers to the study of normal mechanisms and their interactions in regards to the human body. When we talk about physiology of diastole, we are referring to how the heart operates during diastole in a normal situation. It is key we understand the basis of the physiology in order to have a better understanding of abnormal situations.
Diastole occurs in order for the left ventricle (LV) to fill adequately with enough blood, at a low enough pressure, to prevent pulmonary congestion from occurring. This process is referred to as, diastolic function.
The left ventricle has two main jobs that rotate throughout the cardiac cycle:
When we talk about diastolic function, we are evaluating 2 items:
Diastole begins once the aortic valve closes. Let’s recall the 4 stages of diastole:
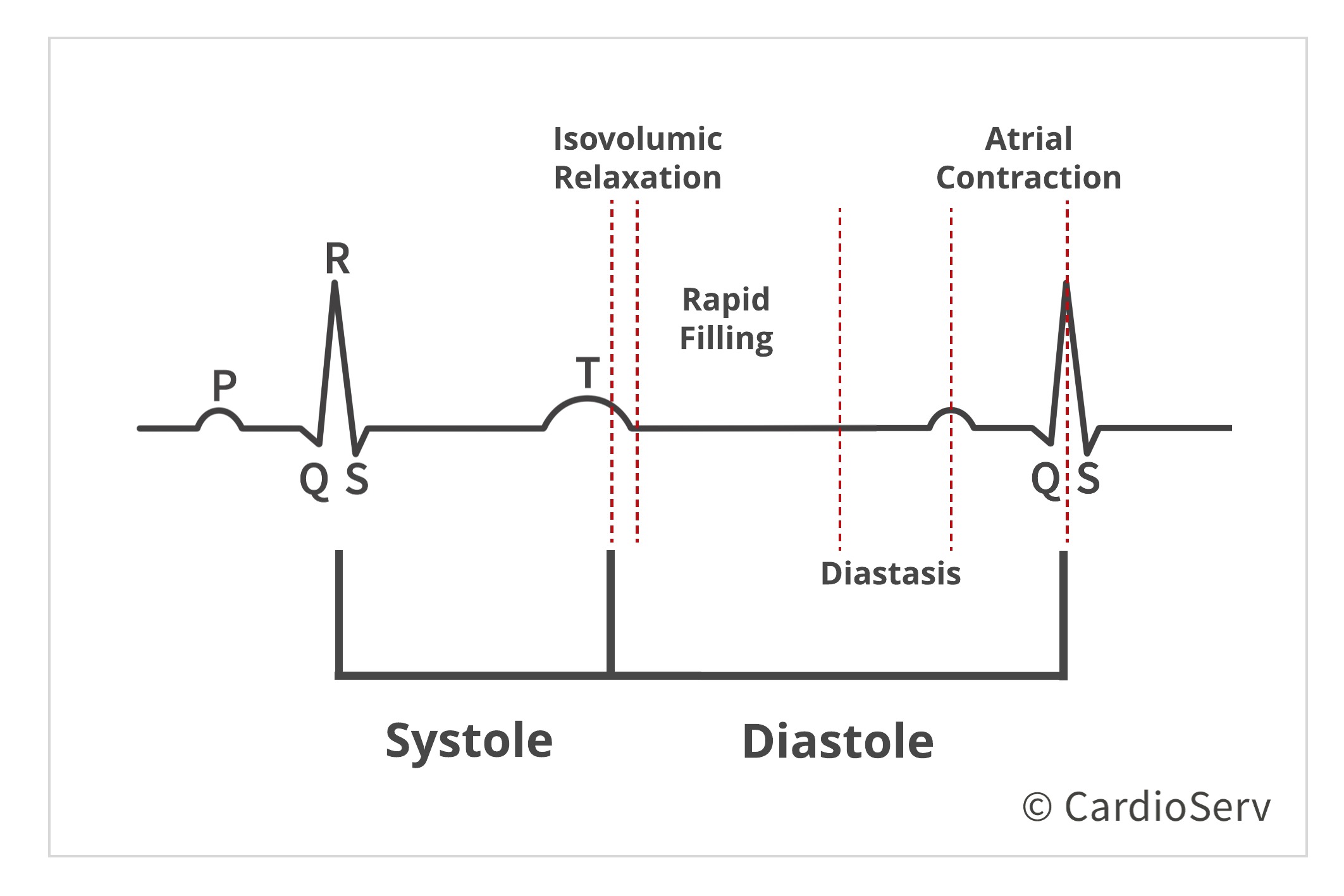
Let’s review what occurs during these stages:
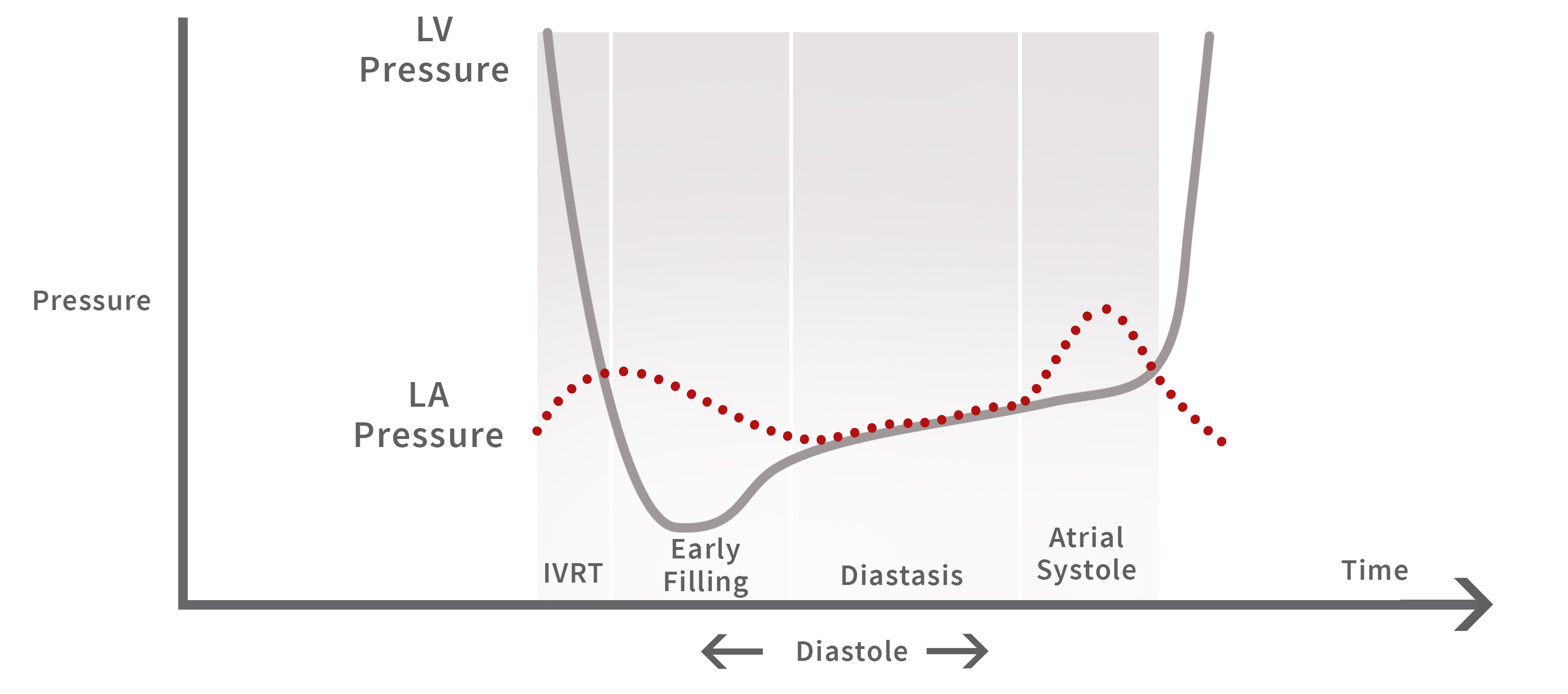
Stage 1- Isvolumic Relaxation: Stage where the aortic valve closes, before mitral valve opens. LV pressure rapidly decreases, without change in volume, to below the LA pressure (LAP). The rate of pressure falling below LA allows the mitral valve (MV) to open (dΔp/dt).
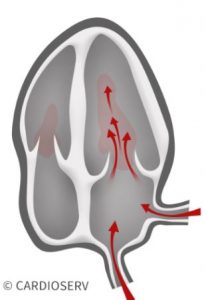
Stage 2- Rapid Filling: Once the MV opens, rapid filling of blood is suctioned towards apex of LV from the LA.
Stage 3- Diastasis: After initial filling of blood, the pressures in both LV & LA equalize and that limits the flow into the LV.
Stage 4- Atrial Contraction: The latest stage of diastole produces a second quick pressure gradient between chambers that pulls the additional blood into the LV.
If disturbance within these 4 stages occurs, preventing the normal process of diastole, a pathophysiological display of diastolic dysfunction will occur. This is why it is essential we cover the normal physiology of diastole, in order to properly evaluate abnormal behavior of diastole.
Knowing the basic process of what occurs during the stages, we need to now understand how these phases occur:
Diastole is composed of both active and passive processes.
Let’s image the heart throughout the cardiac phase:
During systole, the myocardium is being twisted and compressed to eject blood out of the ventricle. When we use the word ‘twisted’ in reference to the LV during systole, think of a mop. When you wring out the mop in the bucket, the closing force twists the bundles of strings to expel the water out. This twisting motion is comparable to the motion of the ventricle. As the LV contracts during systole, it also twists to expel the blood out. During this phase, it allows potential energy to be stored.
Once the aortic valve closes, starting the isovolumic relaxation phase of diastole, the potential energy that was stored during systole gets released. This energy allows the elastic recoil of the ventricle to return to it’s original length and elasticity. Think of a stress ball in regards to elastic recoil- after squeezing the stress ball, we release our grip to allow the ball to return to its original shape.
The process of the myocardium transitioning from a contracted state to its unstressed length and elasticity, demonstrates myocardial relaxation. Relaxation begins at the isovolumic relaxation phase, once the aortic valve closes, and ends at the rapid filling phase.
Relaxation influences the ability of the ventricle to fill properly during diastole. This active process is energy dependent and can easily be impacted by LV disease states, by being delayed or incomplete. For example, if the patients heart rate is high, diastole will be shortened which gives the heart even less time to relax.
The amount of filling during diastole is determined by the compliance (elasticity) of the ventricle and the pressure gradients during diastole. In regards to the physiology of diastole, the normal process refers to how compliant the ventricle is. This passive process begins at rapid filling and ends at the end of diastole.
Compliance is a measure of change in volume relative to change in pressure. A compliant heart can increase its volume without a significant change in pressure. Remember, the goal of diastole is the ability of the ventricle to fill with enough blood at a low enough pressure to prevent pulmonary congestion.
A way to describe the ventricle not being compliant, is to explain the stiffness of the ventricle. Compliance is inversely related to stiffness.
Stiffness is a measure of change in pressure relative to change in volume. A stiff heart will increase in pressure above a normal level to allow a larger volume. Let’s recall- the goal of diastole is to accept volume at a low enough pressure state. If the ventricle is stiff, being abnormal, the pressure will be abnormally high for the amount of volume.
When the ventricle fills, pressure gradients between the ventricle and atrium occur. The gradients represent the end-diastolic pressure (LVEDP) and the mean left atrial pressure (LAP). The LVEDP and LAP can be determined by evaluation of transmitral flow, displaying both rapid filling and atrial contraction phase. These waveforms are demonstrated by the E and A-wave when we pulse-wave Doppler the mitral valve tips.
We evaluate these pressures to determine if they are normal or elevated. This allows us to see the compliance of the ventricle and the ability of the blood to be suctioned towards the apex of the LV from LA, by the rate of blood across the valve.
The filling pattern displayed on the transmital waveform is determined by the relaxation and passive properties of the LV during diastole. When we talk about diastolic function and evaluating the normal process, we must understand the difference between determining the diastolic function and filling pressures.
Diastolic dysfunction refers to the change in filling properties (impaired relaxation, chamber stiffness/compliance).
Increase LV filling pressures will occur secondary due to chamber stiffness. The stiffer the heart, the higher the pressures will increase in order for the ventricle to suction the proper amount of blood for cardiac output.
Elevated diastolic filling pressures is strong evidence for well-developed diastolic dysfunction. We are able to determine filling pressures and grade of diastolic function easily by simple echo parameters.
Now that we understand the stages and physiology of diastole, we understand the importance of this required evaluation method when performing echocardiograms! Next week we will cover general measurements used for examination of diastolic function.
 Andrea Fields MHA, RDCS
Andrea Fields MHA, RDCS
Stay Connected: LinkedIn, Facebook, Twitter, Instagram
References:
Gillebert, T. C., Pauw, M. D., & Timmermans, F. (2013). Echo-Doppler Assessment of Diastole: Flow, Function and Hemodynamics. Education in Heart, 99, 55-64. Retrieved November 20, 2017, from https://pdfs.semanticscholar.org/deda/8ed40076f7bbb1da2668d190d15af9947c2d.pdf.
Nagueh, S. F., MD, Smiseth, O. A., MD, & Appleton, C. P., MD. (2016). Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and European Association of Cardiovascular Imaging. American Society of Echocardiography, 29(4), 277-314. Retrieved October 31, 2017, from http://asecho.org/wordpress/wp-content/uploads/2016/03/2016_LVDiastolicFunction.pdf
Andersen, O. S., MD, Smiseth, O. A., MD, & Dokanish, H., MD. (2017). Estimating Left Ventricular Filling Pressures by Echocardiography. Journal of the American College of Cardiology,69(15), 1937-1948. Retrieved November 29, 2017.
Mitter, S. S., MD, Shah, S. J., MD, & Thomas, J. D., MD. (2017). A Test in Content: E/A and E/e’ to Assess Diastolic Dysfunction and LV Filling Pressures. Journal of the American College of Cardiology,69(11), 1451-1464. Retrieved November 29, 2017.




Dec
2017
Dec
2017
Dec
2017
Jun
2020