Over the past couple weeks, we have broken down essential information needed in order to properly understand and visualize the mitral apparatus. If you haven’t checked it out yet, you can find them:
Let’s review a few important items…
- Examination of the mitral valve (MV) includes all structures that make up the apparatus
- Visualization of the scallops within an imaging window are dependent upon angulation and placement of transducer
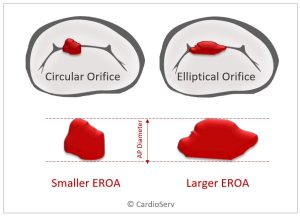
For the blog this week, we are going to cover mitral regurgitation (MR) mechanisms! Our goal for this blog is to be able to identify the type of mechanism causing the MR.
Being able to properly identify the mechanism causing the MR is crucial and mandatory in order to properly determine whether the patient will go for a valve repair, replacement, or be treated medically.
MECHANISMS OF MR
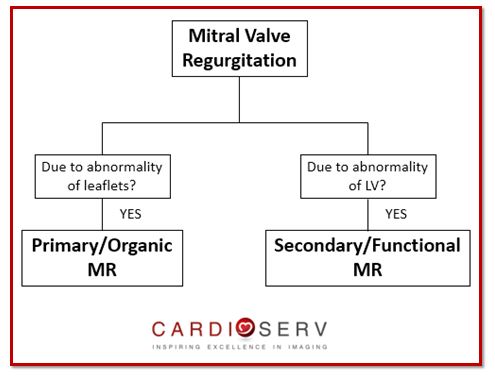
There are 3 different categories that mitral pathology can fall under:
- Organic (Also called Primary)
- Functional (Also called Secondary)
- Mixed Etiologies
Let’s break down each one to better understand!
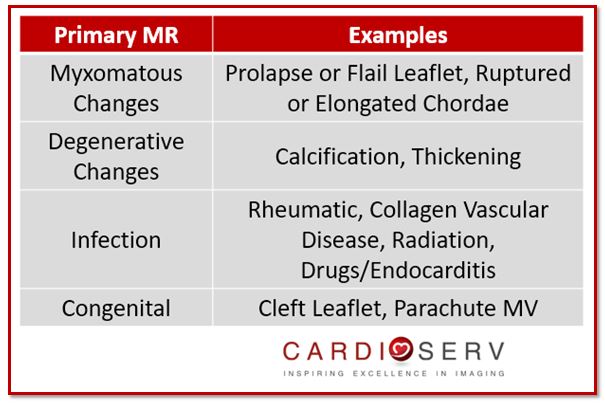
ORGANIC/PRIMARY MECHANISMS
Pathology that falls under organic or primary mechanism indicates pathology is due to abnormality of the mitral leaflets that are causing the mitral regurgitation (MR). Etiologies that fall under this category include:
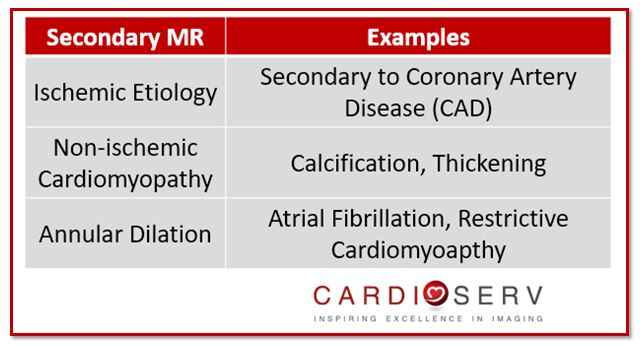
FUNCTIONAL/SECONDARY MECHANISMS
Pathology that falls under functional or secondary mechanism indicates the pathology is due to disease of the left ventricle (LV), not due to the mitral leaflets. Etiologies include:
Use this algorithm to help you determine if the MR is primary/organic or secondary/functional!
MIXED ETIOLOGIES
The ASE does a great job at explaining the importance of documenting mixed etiologies (patient has both primary and secondary mechanisms) in cases when present. If a patient now has severe regurgitation but had only mild a month before-we need to be able to document that the regurgitation is not necessarily new but has worsened due to specific new incident. When would this ever be the case? Let’s break down some examples:
Example 1:
• Patient has chronic ischemic cardiomyopathy with moderate MR
• Patient has acute rupture of chordae tendinae with a flailed MV leaflet causing severe MR
The patient’s history of MR is not a new occurrence, since they have a history of secondary MR. With the new onset of a ruptured chordae causing the leaflet to flail and create now severe MR, that is classified as primary MR. Therefore, in the report, we should document both etiologies. An example may look something like this:
- Patient has history of moderate secondary MR due to chronic ischemic cardiomyopathy.
- Patient presents with now severe MR due to primary acute rupture of chordae causing flail MV leaflet.
Example 2:
• Patient has history of mild primary MR due to mitral valve prolapse (MVP) that is currently being followed by a Cardiologist
• Patient has STEMI and develops moderate to severe MR from MV leaflet tethering
The patient has a known documented history of primary mild MR with mild MVP. Since the patient had a STEMI, it caused the leaflets to tether and worsen the severity of MR. Again, in the report, we should document both etiologies. An example may look something like this:
- Patient has history of primary mild MR due to MVP.
- Patient is s/p STEMI which lead to MV leaflet tethering, causing secondary moderate to severe MR.
SUMMARY
Our goals for this blog were to be able to identify the type of mechanism causing the MR.
Hopefully we are able to grasp the general concept of being able to identify primary/organic from secondary/functional MR. Next week, we will go a step further to classify acute or chronic. This process plays a major role when diagnosing pathology identified on echo! It is also crucial that we report the mechanism of MR as well as acute or chronic.

Andrea Fields MHA, RDCS
Stay Connected: LinkedIn, Facebook, Twitter, Instagram
References:
Zoghbi, W. A., MD, FASE, & Adams, D., RCS, RDCS, FASE. (2017). Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation. JASE, 30, 4th ser., 1-69. Retrieved June 12, 2017.