Diastolic function is a complex process that simply refers to how well the heart performs during diastole, as blood is suctioned from the left atrium (LA) towards the apex of left ventricle (LV) at a low-pressure filling state. When the heart is unable to fill properly, filling pressures increase in order to allow proper filling and keep required cardiac output state. When these filling pressures increase, diastolic dysfunction occurs.
HOW DO WE EVALUATE FOR DIASTOLIC FUNCTION?
The gold standard for determining LV filling pressures, is performed invasively by measuring the left ventricular end-diastolic pressure (LVEDP) via cardiac cath. Another method is by the pulmonary capillary wedge pressure (PCWP), which is an indirect measure of the mean LAP. The mean LAP, obtained via PCWP, correlates to cardiac cath LVEDP. With both of these methods being invasive it is not practical for daily assessment of diastolic function. For this reason we use echo as a non-invasive way to indirectly assess LV filling pressures via LAP by combination of indexes. Echo is a great method because it allows reproducibility on the same patient, which allows us to compare prior findings.
When reporting the diastolic function of a patient via echo, we can report:
- LV filling pressures (normal, elevated or cannot be determined)
- Grade of diastolic dysfunction
- If available, comment on any change from prior studies
By reporting these items, studies have shown to have independent and increasing prognostic information in several settings including heart failure and acute myocardial infarction.
HOW DOES ECHO EVALUATE DIASTOLIC FUNCTION?
Elevated filling pressures are the main consequence of diastolic dysfunction. Remember, if the ventricle is stiff and not compliant, it is unable to fill properly at a low-pressure filling state. In order to allow proper amount of filling during diastole, the filling pressures increase. The ASE recommends determining the grade of diastolic function based on the presence or absence of elevated LV filling pressures.
We are able to evaluate the grade of diastolic function and filling pressures by a combination of parameters.
PARAMETERS OF DIASTOLIC FUNCTION:
- Mitral Annular Velocity
- Transmitral Flow Velocity
- Left Atrial Volume Index
- Tricuspid Regurgitation Velocity
Let’s break down these down in how they play a physiologic role in diastolic function.
MITRAL ANNULAR VELOCITY
Tissue Doppler imaging allows us to evaluate the lengthening of the mitral annuls. During systole, the ventricle contracts and twists towards the apex to eject blood out of ventricle. Once diastole begins, the elastic recoil of the ventricle lengthens to original state. This longitudinal motion of the ventricle lengthening to its original state occurs before filling (in a normal patient). This method evaluates the longitudinal motion and velocity of both myocardial relaxation and restoring forces during rapid filling and atrial contraction phase. In other words, tells us how compliant the ventricle is during diastole.
The Doppler signal displays 3 waveforms:
- S’ : systolic velocity
- e’ : early diastolic velocity
- a’ : late diastolic velocity
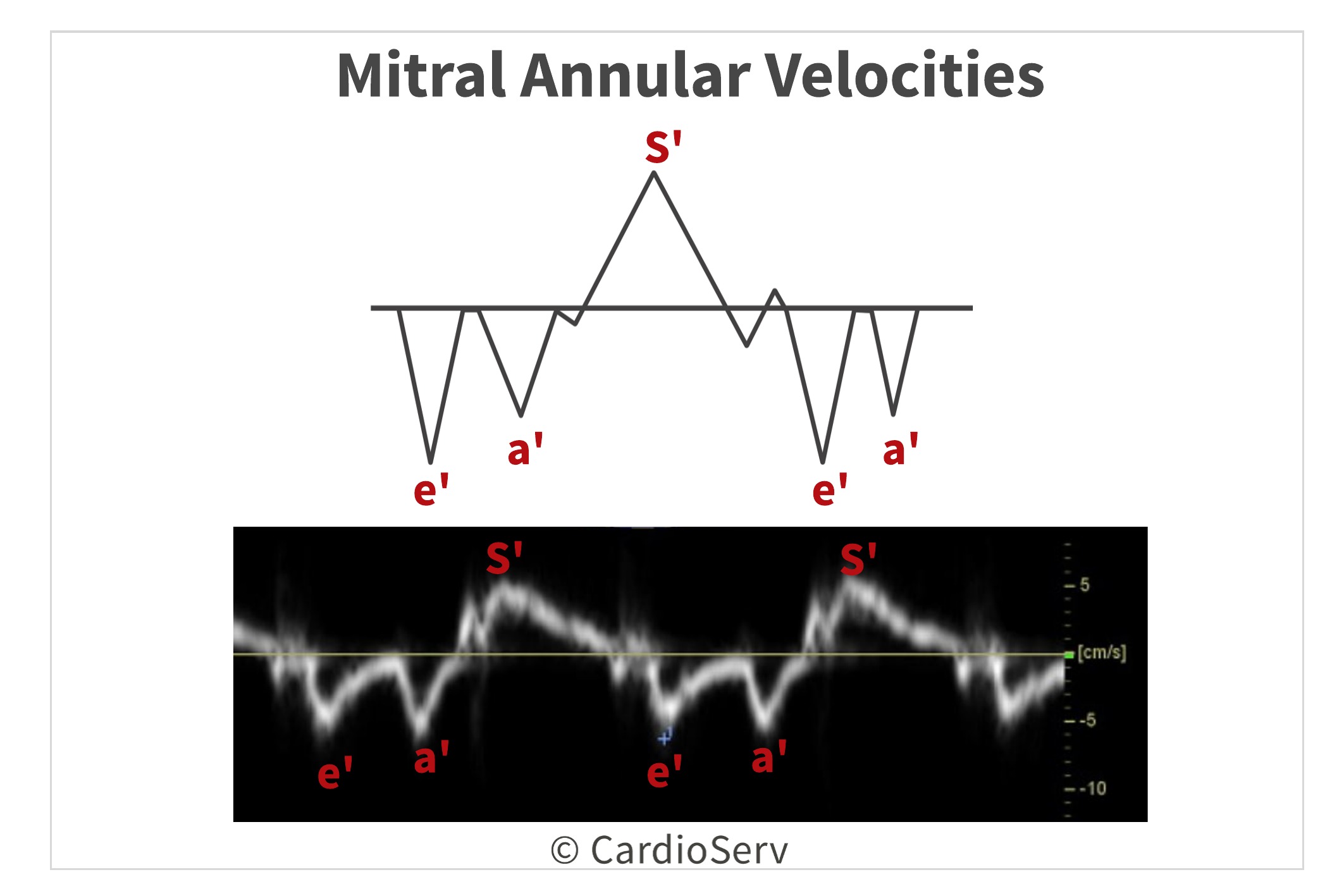
The e’ velocity corresponds with early rapid filling and the a’ velocity corresponds with atrial contraction.
ITEMS TO CONSIDER:
- Basal regional wall motion abnormalities can alter velocities
- Right heart pathology or pulmonary hypertension can affect septal velocities
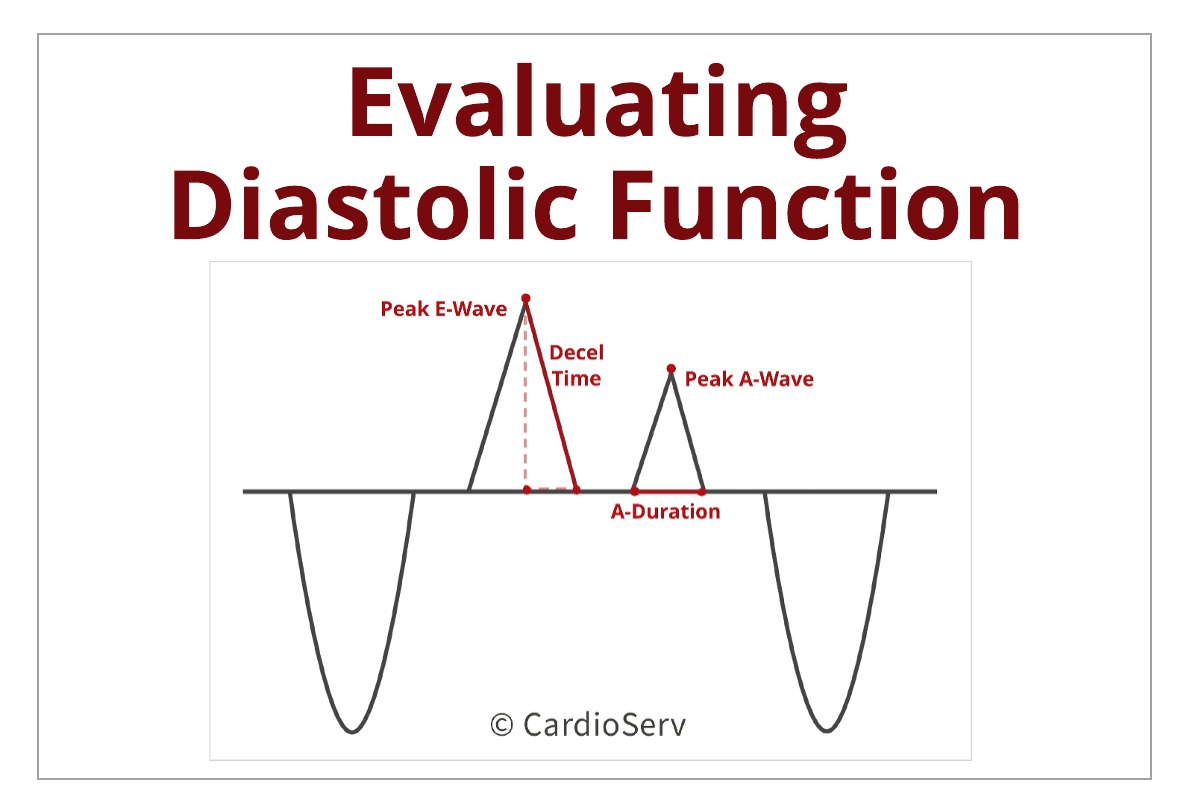
TRANSMITRAL FLOW VELOCITIES
Transmitral flow velocities gives us insight to the LV filling pressures. The velocities are determined by the transmitral pressure gradient, which correlates with the peak transmitral filling rate (velocities).
The Doppler signal displays:
- E-Wave: peak early filling velocity (rapid filling)
- A-Wave: late diastolic filling velocity (atrial contraction)
- E/A Ratio
- A-Duration: time interval between onset and ending of A-Wave
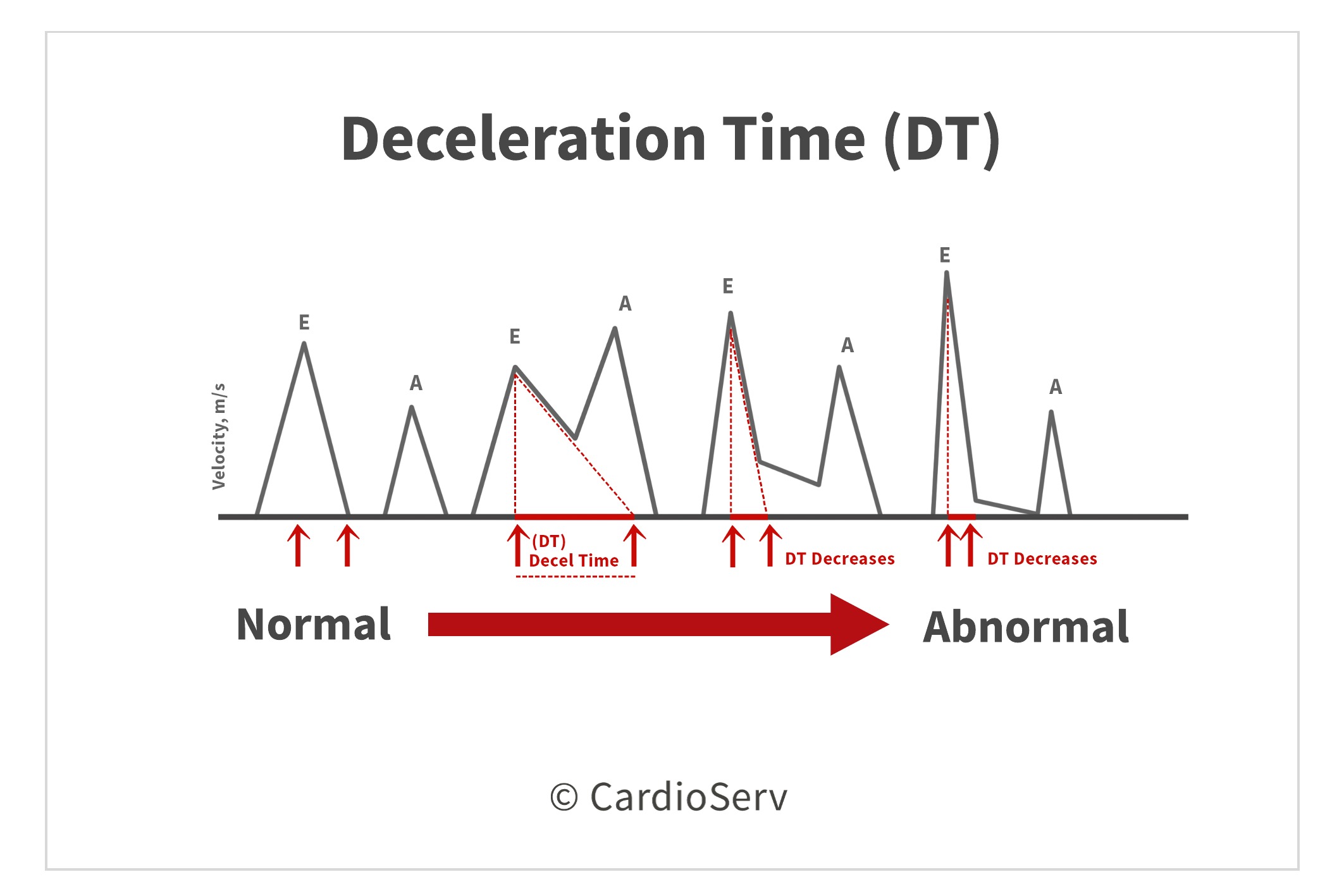
- Deceleration Time (DT): early filling velocity
- Isovolumic Relaxation Time (IVRT): time interval between aortic closure and mitral opening
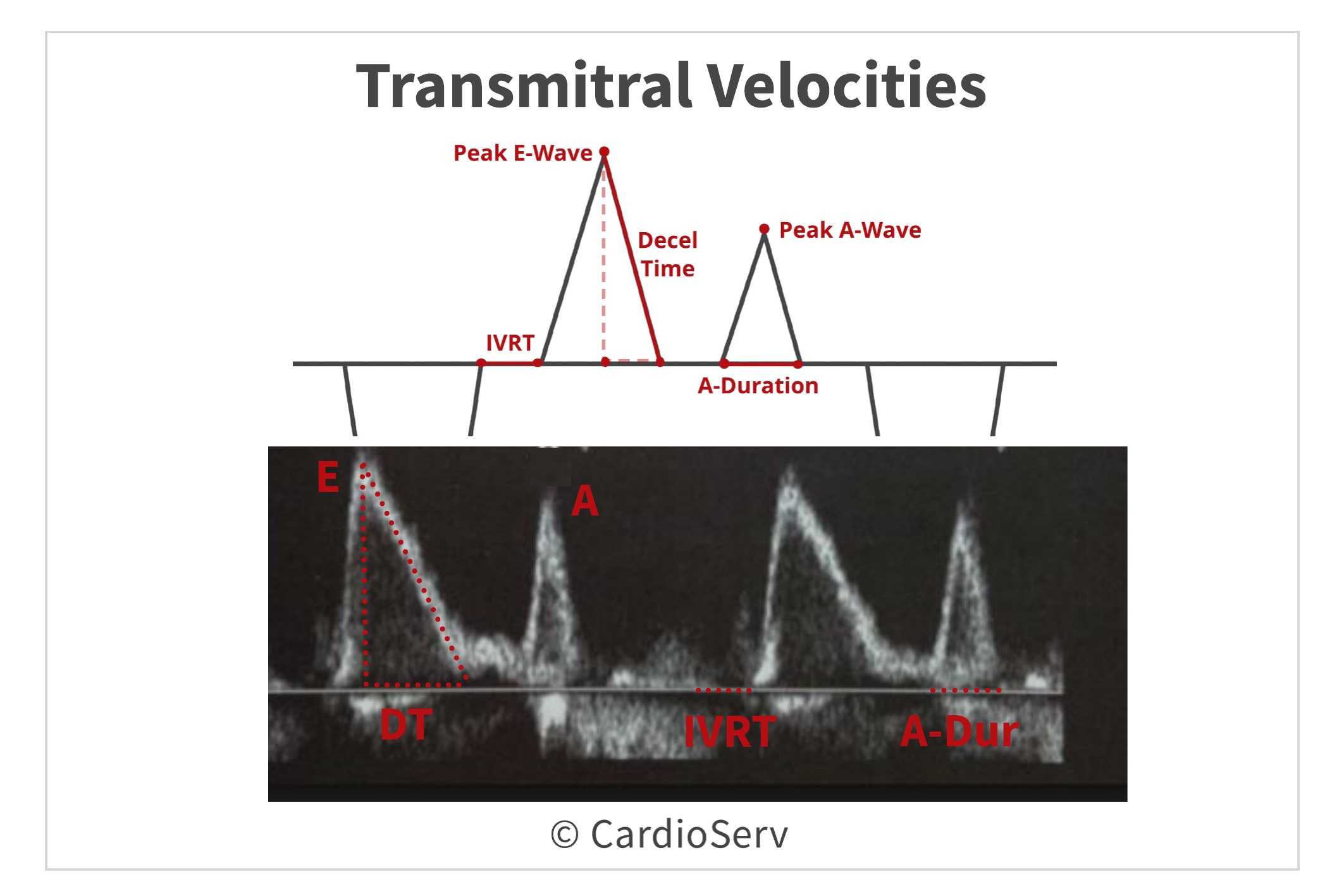
The E-wave velocity reflects the LA and LV pressure gradient during early diastole. This allows the mitral E-wave velocity can be a good reflector of the estimation of left atrial pressure (LAP) and rate of LV relaxation. Changes in the E-wave can also be an alert of changes in the filling pressures.
The A-wave velocity is reflective of the LA and LV pressure gradient during late diastole. Remember, this is the stage of diastole where atrial contraction occurs. Therefore, the velocity represents how well the last stage of diastole is performing.
The E/A ratio is a key measure when we evaluate for diastolic function. The E-wave represents early rapid filling and the A-wave represents atrial contraction. The ratio and pattern suggests if the diastolic filling is occurring at the proper time and rate during diastole. In the early stages of diastolic dysfunction, there will be a decrease of early rapid filling with an increase in atrial contraction, to compensate for the lack of filling in the first phase. This ratio provides both prognostic and diagnostic information.
The A-Duration measurement is reflective of the time the atrial contraction phase occurs. This is the last phase of diastole and should normally be a short period of time.
The Deceleration Time (DT) can provide us valuable information as well! As blood moves across the mitral valve, the LAP decreases and the LV pressure increases. Once the pressures equalize, blood flow stops. We are able to determine the rate of time from peak to zero-baseline of the mitral E-wave velocity. This time interval is influenced by the compliance and pressures of the LV. For example: the stiffer the ventricle (less compliant), the shorter the DT time will be.
The Isovolumic Relaxation Time (IVRT) is the duration of ventricle relaxation during first stage of diastole. When relaxation is delayed or prolonged (elevated filling pressures), this causes the timing of mitral valve to open later. When this happens, the IVRT is increased, or has a long occurrence time. On the other hand, IVRT will be shortened when the LAP is elevated, causing the mitral valve to open earlier than normal. Therefore IVRT is inversely related to the LAP and directly related to LV filling pressures.
ITEMS TO CONSIDER:
- Transmitral velocities are heart rate & abnormal conduction system dependent: arrhythmias
- In the presence of atrial fibrillation: A-wave will not be present
- Transmitral velocities are age dependent: velocity will decrease with advancing of age
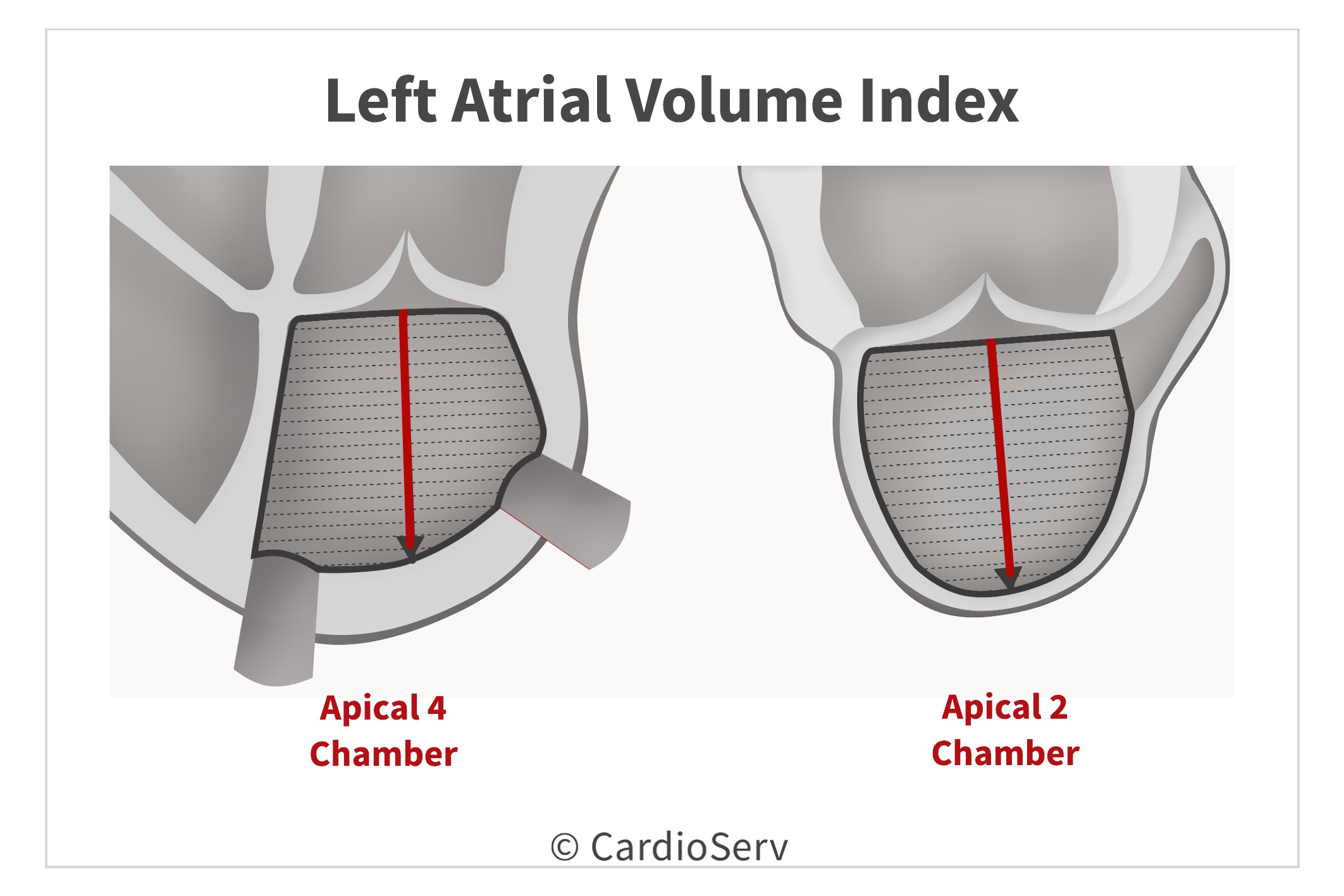
LEFT ATRIAL VOLUME INDEX
Left atrial enlargement is a key marker of long-standing elevated left atrial pressure (in cases without chronic atrial arrhythmias). The volume is indexed to BSA to properly scale accordingly to body size. There is strong data that reflects the relation between chamber remodeling to diastolic dysfunction. A dilated atrium is an independent predictor of cardiovascular complications, such as death, heart failure, atrial fibrillation and ischemic stroke. It also has prognostic information on the chronicity and degree of diastolic dysfunction.
TRICUSPID REGURGITATION VELOCITY
The final echo parameter for evaluating diastolic function is peak TR velocity. Elevation of pulmonary artery pressures provides insight to LV filling pressures and will be discussed in later blogs. In echo, we can determine the pulmonary artery pressures by measuring the peak velocity of the tricuspid regurgitation (TR) jet. When there is no pulmonary disease present, an increased TR jet > 2.8 m/sec is suggestive of an elevated LAP.
SUMMARY
Now that we have a basic understanding of the physiology that determines the evaluation of diastolic function, we can efficiently use the ASE’s algorithm! Next week, we are going to discuss how the presence of diastolic dysfunction alters the normal physiology of diastolic function.

Andrea Fields MHA, RDCS
Stay Connected: LinkedIn, Facebook, Twitter, Instagram
References:
Gillebert, T. C., Pauw, M. D., & Timmermans, F. (2013). Echo-Doppler Assessment of Diastole: Flow, Function and Hemodynamics. Education in Heart, 99, 55-64. Retrieved November 20, 2017, from https://pdfs.semanticscholar.org/deda/8ed40076f7bbb1da2668d190d15af9947c2d.pdf.
Nagueh, S. F., MD, Smiseth, O. A., MD, & Appleton, C. P., MD. (2016). Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and European Association of Cardiovascular Imaging. American Society of Echocardiography, 29(4), 277-314. Retrieved October 31, 2017, from http://asecho.org/wordpress/wp-content/uploads/2016/03/2016_LVDiastolicFunction.pdf
Andersen, O. S., MD, Smiseth, O. A., MD, & Dokanish, H., MD. (2017). Estimating Left Ventricular Filling Pressures by Echocardiography. Journal of the American College of Cardiology,69(15), 1937-1948. Retrieved November 29, 2017.
Mitter, S. S., MD, Shah, S. J., MD, & Thomas, J. D., MD. (2017). A Test in Content: E/A and E/e’ to Assess Diastolic Dysfunction and LV Filling Pressures. Journal of the American College of Cardiology,69(11), 1451-1464. Retrieved November 29, 2017.