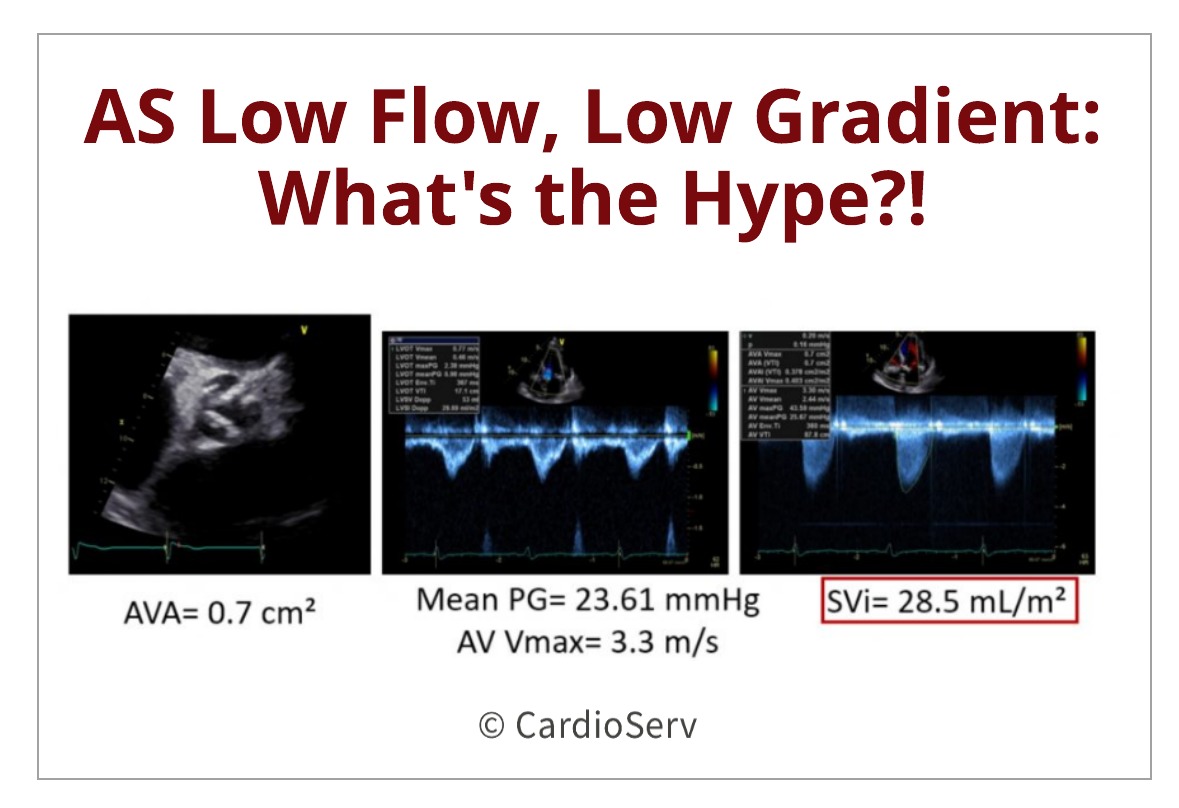
We’ve all been in this situation…. our patient appears to have a very tight, calcified aortic valve which visually appears to be moderate to severe aortic stenosis. As we scan through our protocol, we obtain a peak aortic valve velocity of 3.3 m/s and mean pressure gradient (PG) of 23.6 mmHg. The calculated AVA is showing 0.7cm², but the obtained velocity values do not add up to the severely indicated AVA? What could be causing this? Is this correct? Does the patient have moderate or severe AS?
It is important as clinicians to understand the hemodynamics and methodology of calculating the aortic valve area using the continuity equation. It is common to experience discordant values that do not match the textbook explained method. This blog is going to discuss two situations that commonly occur: low-flow, low-gradient aortic stenosis with reduced and preserved LV EF.
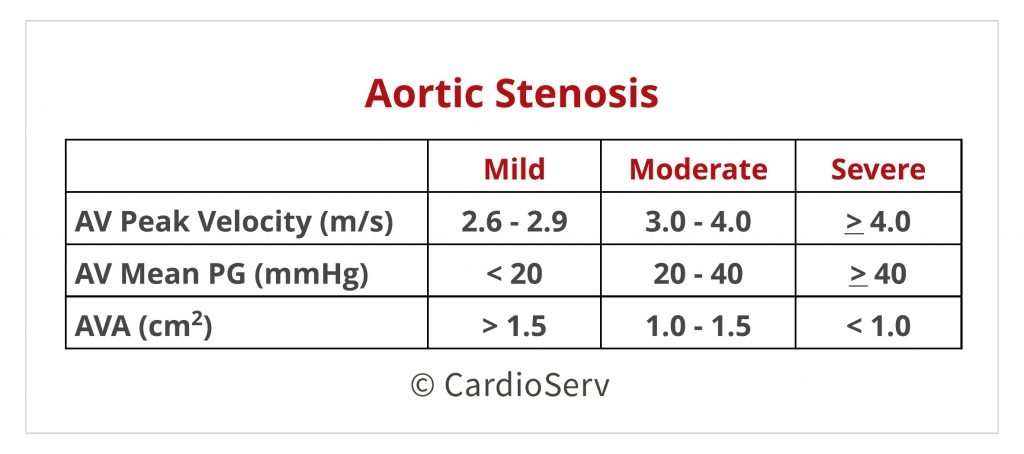
PARAMETERS FOR SEVERE AORTIC STENOSIS
First, let’s cover the basic parameters for severe aortic stenosis:
- AV Max Velocity > 4 m/s
- AV Mean PG > 40 mmHg
- AVA < 1.0 cm²
- Dimensionless Index < 0.25
Any one of these parameters can suggest severe aortic stenosis, however there should be concordance between all parameters!
DISCORDANT AORTIC STENOSIS PARAMETERS
There are situations where our severity cut-off parameters do not match up like we wish they would….
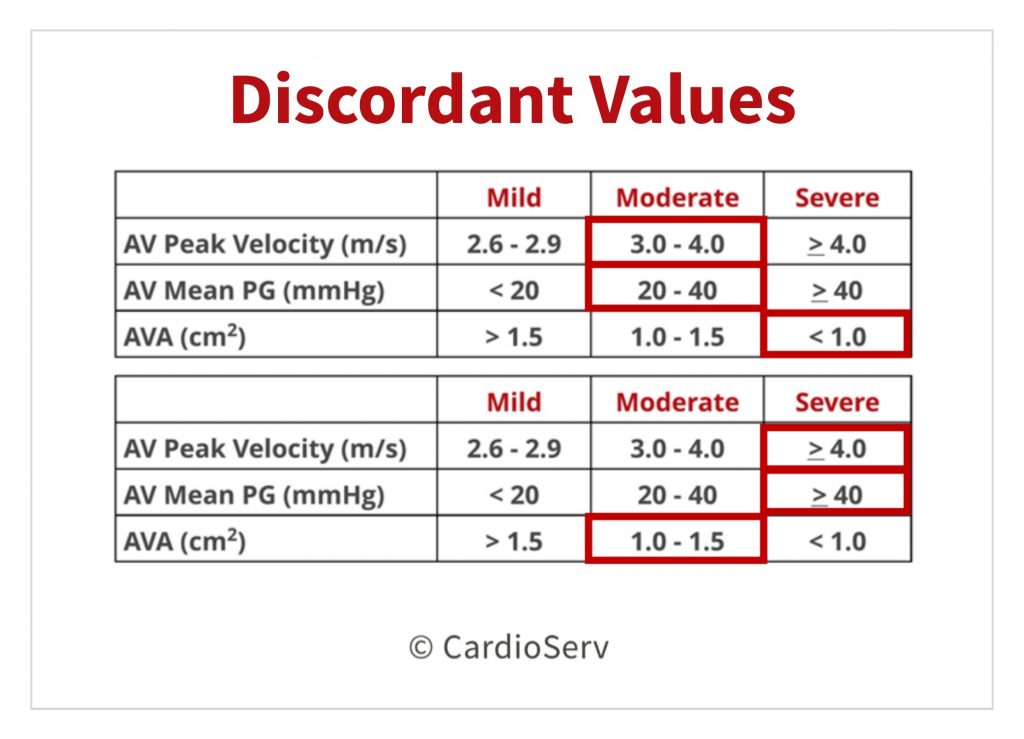
What do we do when the gradient/velocity do not correlate with the AVA severity parameters….. FURTHER INVESTIGATION!
STEP 1: RULE OUT ERRORS!
The first and most important part is to rule out potential measurement errors! This includes all parameters involved in the continuity equation:
- LVOT Diameter
- LVOT VTI Velocity
- AV Peak/Max VTI Velocity
STEP 2: CONSIDER OTHER ENTITIES!
After you are able to confirm there are no errors in the measurements, then we can move forward to considered other types of aortic stenosis:
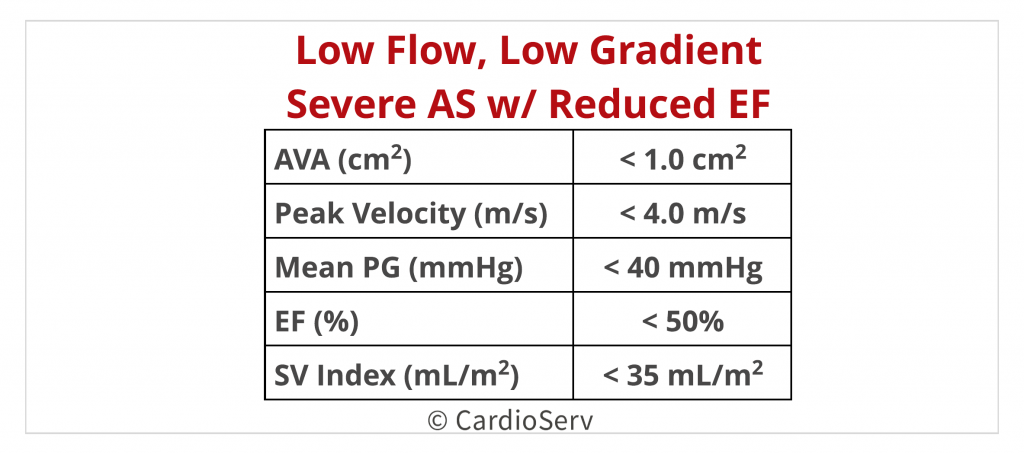
- Low Flow, Low Gradient with Reduced LV EF
- Low Flow, Low Gradient with Preserved LV EF
WHAT’S THE HYPE?!
What is the hype about these two? What makes the outcome different based on the ejection fraction? Let’s talk this through….
- The term “Low Flow, Low Gradient” — remember velocity/gradients are FLOW DEPENDENT!
- Flow Status = Stroke Volume Index (SVi) < 35 mL/m²
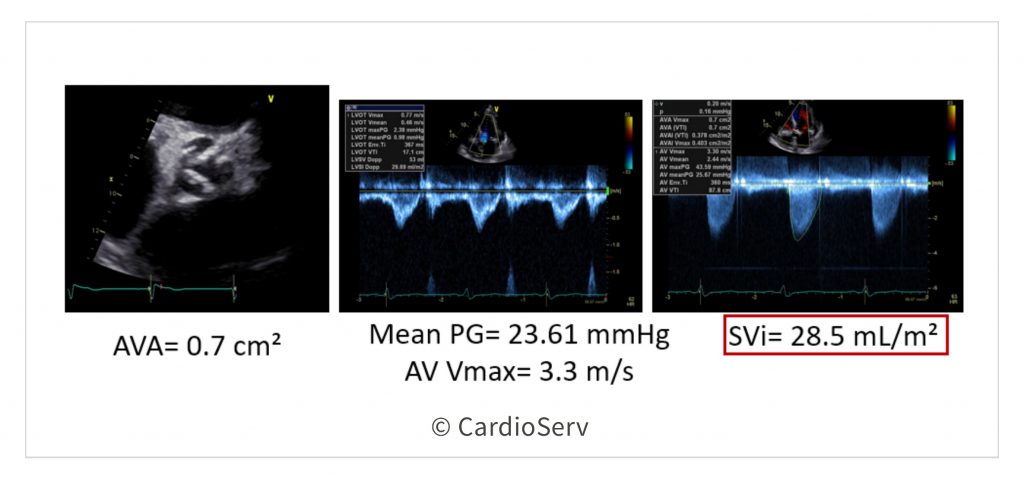
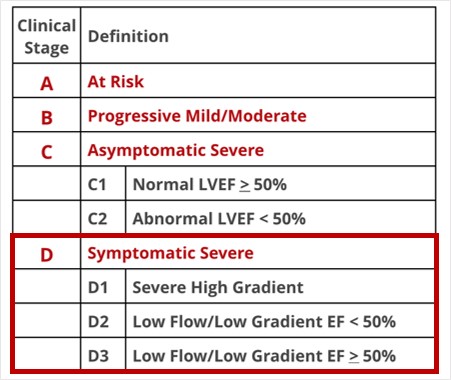
The stroke volume is low (< 35 mL/m²), velocity/gradients are low ( <4 m/s & <40 mmHg), but the AVA is displaying as SEVERE (< 1.0 cm²). Depending on the ejection fraction (reduced vs. preserved) will guide us to different questions.
PRESERVED EF > 50%
If the EF is preserved (> 50%) , we need to look at a few potential factors contributing to these findings:
- Reason #1: ERROR …… take another look back at your measurements, are you POSITIVE you did not over/under measure the LVOT diameter?
- Reason #2: What type of patient is this?
A lot of times when we have elderly (>70 years old) small bodied patients, they commonly have small LV cavities (low volumes) and LVH (commonly due to chronic hypertension). This will cause a decrease in the gradient/velocities because of the low flow volumes and not much volume to pump out of the thickened small chamber.
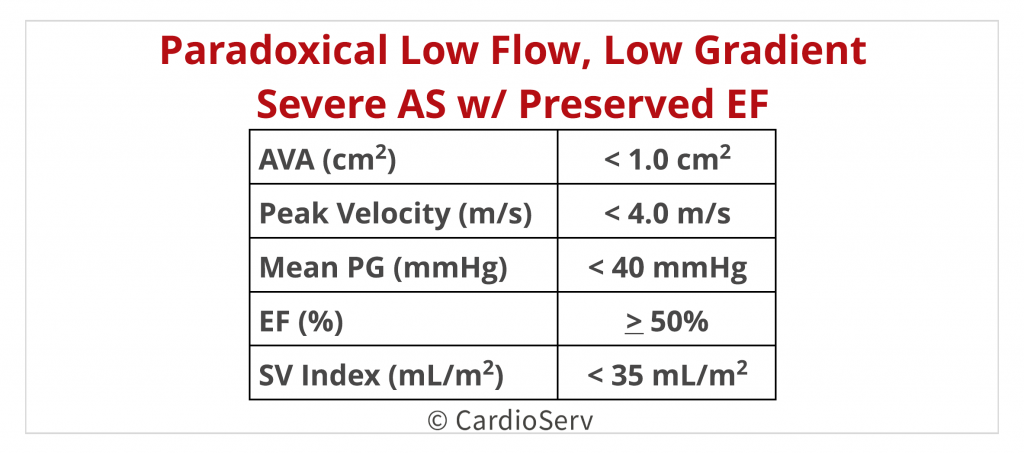
In this situation, the ASE guideline paper recommends using an integrated approach to determining the true severity of the stenosis.
REDUCED EF <50%
First and most important part….. velocity & gradients are FLOW DEPENDENT! In other words, if the EF is decreased then that will affect the velocities and gradients!
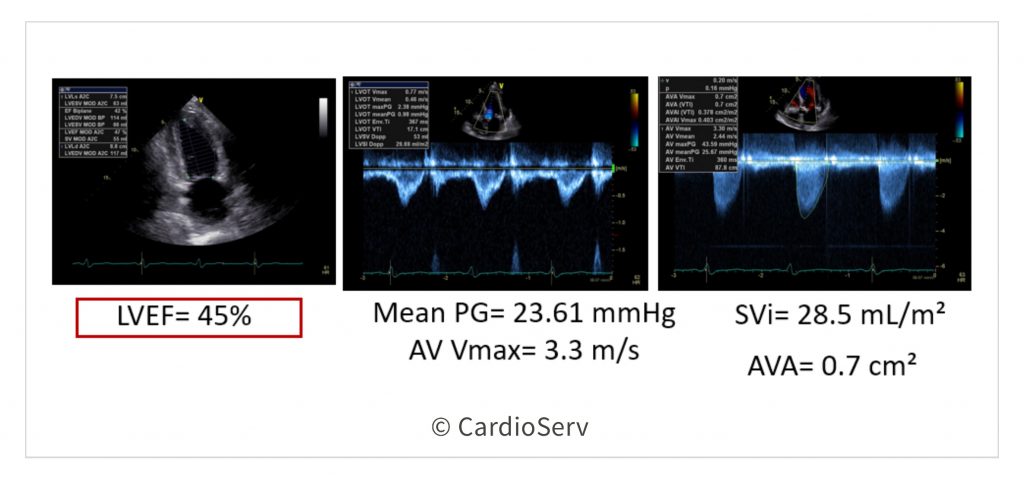
In situations where we calculate an AVA of < 1.0 cm² with low gradient/velocities (< 4 m/s & < 40 mmHg), low flow status (< 35 mL/m²) and a REDUCED EF (<50%) = we MUST take further investigative steps to determine the cause of low flow status with severely calculated AVA!
If the EF is reduced (<50%), then we need to determine if the decrease in valve opening (AVA) is due to true severe AS or LV dysfunction? Low flow status hinders the ability of force applied for the leaflet cusps to open = cause decrease in AVA. What would the gradient/velocity be if the myocardium was functioning at a normal state?
The answer is 3 simple words ….. Dobutamine Stress Echo ! This test allows us to evaluate the heart as if it were function at an increased EF by giving dobutamine! We want to look for:
- Contractile Reverse- contractile response to Dobutamine
- Stroke Volume- Presence of flow reverse (> 20% SVi from baseline)
We can end up with 2 main outcomes…
- Pseduo AS: low flow is causing the velocity/gradients to overestimate the severity of AVA due to LV Dysfunction
- Once the heart was functioning at a normal state (thank you Dobutamine), the valve had enough push power to open at its full capacity… increasing the stoke volume > 20% from baseline & calculated the AVA to > 1.0 cm²
- True Severe AS: severe aortic stenosis is present and causing the LV systolic dysfunction (low flow)
- After giving Dobutamine the velocity/gradients increased, the SVi increased > 20% but the AVA remains < 1.0 cm²
Of course there is always the 3rd outcome of no change in stroke volume (absence contractile reserve). These patients have a high mortality rate due to the myocardium not being viable.
SUMMARY
We all have those patients where our measurements do not all correspond to the severity reference charts. It is vital in these situations we take additional steps to further investigate the reason behind these discordant values.
- Rule out errors! The most common error is in the LVOT diameter.
- Evaluate the patients flow status! Look at the stroke volume index…. is it abnormally low? < 35mL/m²
- What is the LV ejection fraction? Is it preserved (> 50%) or reduced (<50%)?
- Is the < 1.0 cm² AVA due to TRUE severe AS or LV dysfunction?
Incorporating these investigation questions helps provide the best patient care we all strive to provide our patients!
Check out our past blogs on aortic stenosis!
- Top 5 Factors to Consider when Evaluating for AS
- Aortic Stenosis: Breaking Down the Continuity Equation
- 4 Errors to Avoid when Measuring Aortic Valve Velocity
- Helpful Tips to Mastering the Pedoff Probe!
- Back to Basics: Aortic Valve Anatomy
- How to Master Aortic Measurements with These 5 Techniques
- Additional Methods to Evaluating Aortic Stenosis
Want to earn Cat. 1 AMA ECHO CMEs?! Access them HERE!

Andrea Fields MHA, RDCS
Stay Connected: LinkedIn, Facebook, Twitter, Instagram
References:
Baumgartner, H., Hung, J., Bermejo, J., Chambers, J. B., Edvardsen, T., Goldstein, S., . . . Otto, C. M. (2016). Recommendations on the echocardiographic assessment of aortic valve stenosis: A focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. European Heart Journal – Cardiovascular Imaging, 18(3), 254-275. doi:10.1093/ehjci/jew335
Nakatsuma, K., Taniguchi, T., Morimoto, T., Shiomi, H., Ando, K., Kanamori, N., . . . Kimura, T. (2017). Prognostic Impact of Peak Aortic Jet Velocity in Conservatively Managed Patients With Severe Aortic Stenosis: An Observation From the CURRENT AS Registry. Journal of the American Heart Association,6(7). doi:10.1161/jaha.117.005524