As a community committed to inspiring excellence in imaging we thought it would be useful to share some interesting echo case studies so that we can all learn together. Please reach out to us with any interesting studies that you would like to share! Matthew Cox, BS, RDCS from OSF Heathcare in Illinois was kind enough to share an interesting echo case study he was involved with. Learn more about Matt in our Educator Spotlight! His case study includes transthoracic images along with both 2D and 3D TEE images. Follow the case study and see if you agree with the final diagnosis and differential diagnosis. Take it away Matt!
PATIENT HISTORY
This was an 89-year-old Caucasian female patient that arrives via EMS for generalized weakness and fatigue. Her EKG showed normal sinus rhythm despite a history of paroxysmal atrial fibrillation. She had a 2-3/6 systolic murmur that was heard during auscultation.
Vitals:
- BSA is 1.7 m²
- BP 140/72
The patient’s history was as follows:
- Status post aortic valve replacement (AVR)
- Septal Myomectomy due to hypertrophic obstructive cardiomyopathy (HOCM)
- Congestive Heart Failure
- Paroxysmal atrial fibrillation (PAF) – Pt. declined anticoagulation
- COPD
- Dyspnea
- Lymphedema
- Hypertension
- CVA >2 years ago
- Dyslipidemia
ECHO CASE STUDY: TRANSTHORACIC ECHO
Video Player
00:00
00:20
Needless to say the cardiologist ordered a TEE to better evaluate the mitral valve.
ECHO CASE STUDY: 2D TRANSESOPHAGEAL ECHOCARDIOGRAM
Video Player
00:00
00:31
ECHO CASE STUDY: 3D TRANSESOPHAGEAL ECHOCARDIOGRAM
Video Player
00:00
00:36
CASE REVIEW
EIGHTEEN MONTHS EARLIER
Eighteen months earlier the patient had received a #21mm bioprosthetic aortic valve replacement and septal myomectomy due to her Hypertrophic Obstructive Cardiomyopathy (HOCM). At that time her aortic valve velocities were within normal range for a bioprosthetic valve.
SEVEN MONTHS EARLIER
The patient had a routine follow-up echocardiogram that showed progressive mitral stenosis and trace mitral regurgitation. There was no mention of endocarditis or flail leaflet. The aortic valve demonstrated normal bioprosthetic velocities and structure.
TWO MONTHS EARLIER
The patient was hospitalized for acute choledocholethiasis (gallstones). At this time her blood cultures were positive for group B strep. She was given Zosyn which was later changed to Unasyn. Repeat blood cultures were negative.
TWO WEEKS PRIOR
The patient was doing well until her energy level dropped acutely. Her urine was tested despite no urinary symptoms and grew Enterobacter. She was started on Omnicef which she took for 7 days. Her energy level did not improve with Omnicef.
HOSPITAL ADMISSION
1. Transthoracic Echo
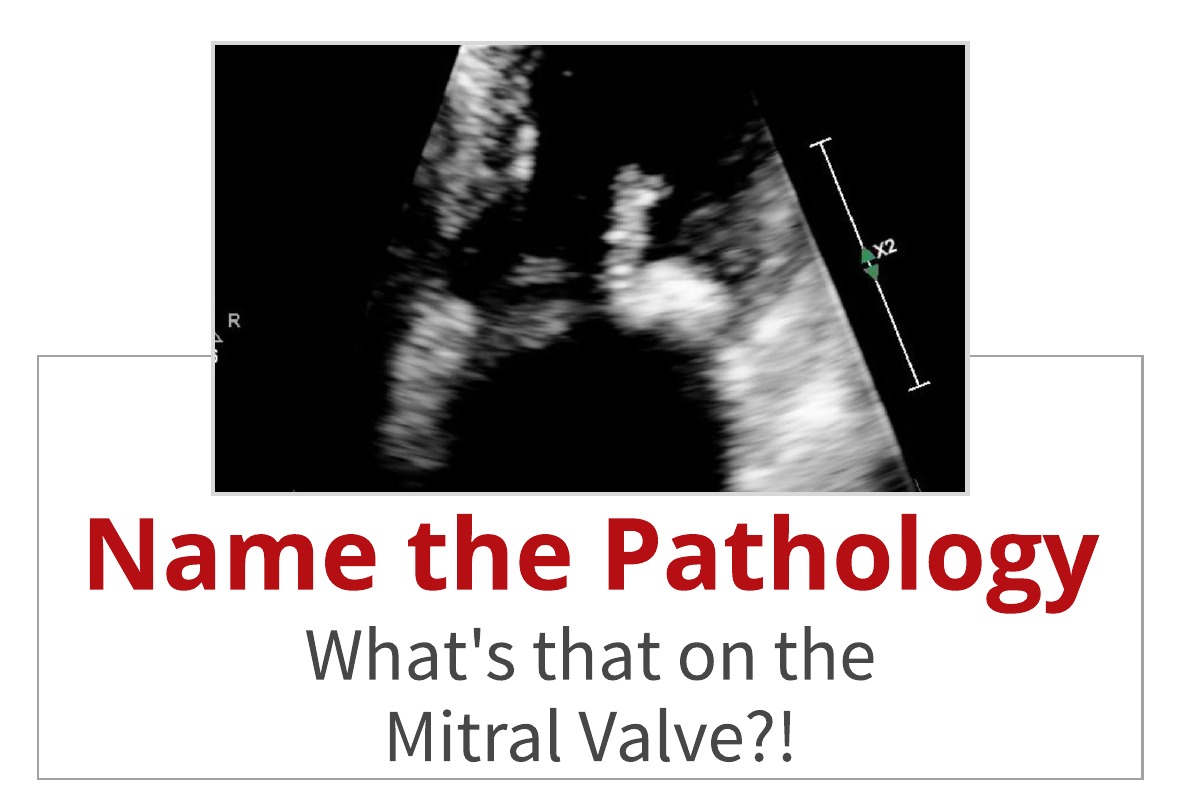
An echo was performed and showed a large, mobile, irregular mass attached to anterior mitral valve leaflet that measured 0.8cm x 1.0 cm.
Differential diagnosis: Vegetation, flail leaflet versus calcification.
Blood cultures were drawn and she was started on Vancomycin and Zosyn. Blood cultures came back negative for any growth.
2. Transesophageal Echo
The TEE findings included:
• A linear, mobile, hyperechoic structure noted on the atrial aspect of posterior mitral leaflet, on P1 scallop/posterior annulus junction with independent motion.
• Mild central mitral regurgitation.
• Echo dense structure measured 2.15cm x 1.0cm
Differential diagnosis: Healed vegetation covered with thrombus vs papillary fibroelastoma (given recent cardiac surgery as trauma could be a risk factor for the growth of papillary fibroelastoma) vs large calcification covered in thrombus. Does not appears as acute vegetation based on echogenicity, however clinical correlation is required.
3. Cardiac MRI
Cardiac MRI performed with findings of a markedly limited exam due to patient not tolerating the exam well and ending the exam after 5 minutes. When comparing to CT scan from three years prior (which occurred prior to patient’s aortic valve replacement and septal myomectomy) there is extensive heavy calcification at the mitral valve annulus and posterior leaflet of the mitral valve as well as at the chordal insertion.
Differential diagnosis: The findings on echocardiogram could represent mitral valve annular calcification and calcification of the posterior mitral valve leaflet as well as calcification of the chordal elements at the insertion compatible with the CT scan from 2015 showing extensive heavy calcification in these areas. It would be difficult to exclude myxomatous thickening of the mitral valve leaflets intermixed with calcification. Also would be difficult to exclude a component of a small papillary fibroelastoma mixed with calcification. When correlating with patient’s echocardiogram there is echogenic material which appears mobile on the posterior leaflet of the mitral valve as well as echogenic material related to the mitral valve annulus. The leaflet of the mitral valve on echo appears thickened. There does appear to be some restricted motion of the posterior leaflet.
SUMMARY FINDINGS:
The physician’s final summary after labs, TTE, TEE, and Cardiac MRI were as follows:
It looked like annular calcification on MRI and it makes sense based on the site of attachment. There are documented cases of this in literature. She had surgery for AVR which can disrupt the integrity of the MV annulus. The possibility of healed calcified vegetation is another thought and/or fibroelastoma. Unfortunately, we cannot definitively prove one or the other because the patient’s wishes are no more surgery and a true diagnosis of papillary fibroelastoma requires histology and biopsy of structure which patient is unwilling to agree to. Additionally, acute vegetation can be ruled out by negative lab work.
MOBILE MASS ON MITRAL ANNULUS CALCIFICATION
A case presented in the Journal of Cardiology Cases (volume 6, issue 1) discusses a handful of similar cases. The featured case involved an 80 year old woman with a mobile mass (0.7cm x 0.54cm) on the ventricular side of the calcified mitral annulus of the posterior leaflet. Discussion of the case included some of the following highlights (check out the complete article):
- 19 patients with reports of mobile masses on the MAC
- More common for the mobile mass to arise from the MAC of the posterior leaflet
- More frequently on the atrial side than the ventricular side of the MAC
- “Although the precise mechanisms of the development of the mobile mass on the MAC are unknown, it is possible to postulate that the morphology and the size of the MAC affect the process of the mobile mass formation on the MAC” (Nagai, et al., 2012).
Another case with very similar images to this case can be found here at Science Direct: Mobile thrombus originating from densely calcified mitral annulus with cerebral embolism.
So what do you think? Not all pathology can be diagnosed by just echo alone and we can be left with unanswered questions when a patient does not want additional testing. Do you agree with the diagnosis and/or differential diagnosis? Leave your comments below regarding the mystery of her mitral valve disease.

Matthew Cox, B.S., RDCS
Connect with Matthew on LinkedIn
Reference
Nagai, T., MD, Kusano, H., MD, Hamabe, A., MD, Arakawa, J., MD, Konishi, T., MD, Hisadome, H., MD, . . . Uehata, A., MD. (2012, May 16). Newly developed mobile mass superimposed on mitral annulus calcification in patient with cerebral infarction: Documentation of a unique embolic source. Retrieved from https://www.sciencedirect.com/science/article/pii/S1878540912000229
Have an interesting echo case study? Contact us to submit your case study.