As we continue our blog journey on the topic of mitral regurgitation, we hope you have been able to review our prior educational posts! If not, no worries– you can find them here!
- Mitral Valve Anatomy: Name 5 Components!
- Finally…Mitral Valve Orientation Explained!
- Smart Strategies for Determining MR Mechanisms
Last week, we covered vital information in order to determine the type of mechanism causing the mitral regurgitation (MR). This week, our goal is to take that information one step further and discuss how to:
- Determine if the mechanism is acute or chronic
- How that affects the hemodynamics of the heart
This week we will break down three different hemodymamic stages that can occur in the presence of MR:
- Acute
- Chronic Compensated
- Chronic Decompensated
ACUTE MR
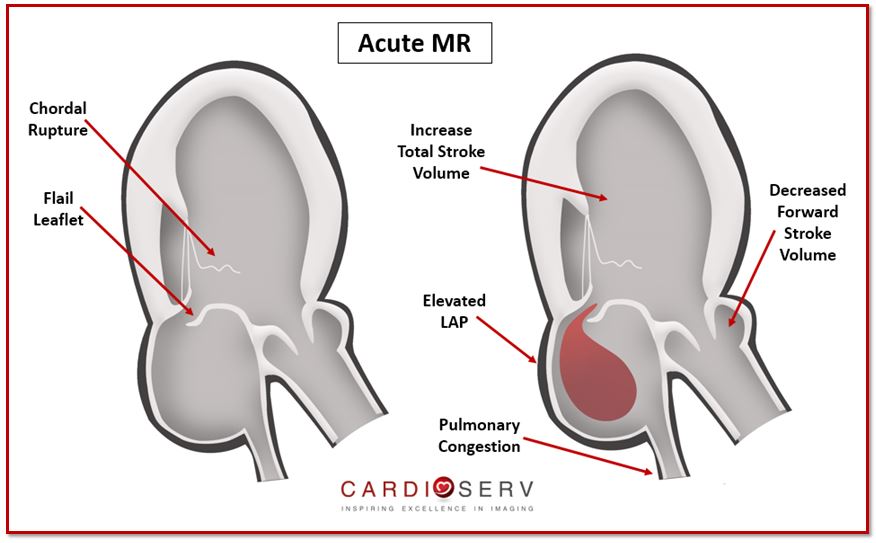
Acute MR can be the result of a flail leaflet, torn papillary muscle or an acute myocardial infarction (MI). Any of these acute changes can cause hemodynamic compromise on the left ventricle and atrium. Remember, it is always more challenging to diagnose acute pathology than chronic due to rapid onset of symptoms, hemodynamics and physics.
When an acute onset of regurgitation occurs, there is a rapid onset of volume overload for the LV & LA. Neither chambers are prepared for this change, which causes chaos within the heart.
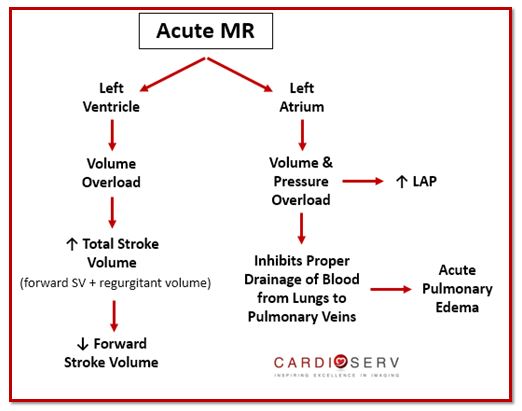
With the extra volume that is being pushed back into the LA during systole, the ventricle has to work extra hard in order to pump out both forward SV plus regurgitant volume. The LA is not compliant with the rapid onset of additional volume, which causes the LA pressure (LAP) to increase. This prevents proper drainage of blood from lungs to pulmonary veins, which causes the development of pulmonary congestion and edema.
This will cause the following signs & symptoms:
- Hypotension
- Dyspnea
- Tachycardia
- Pulmonary Edema
- Palpitations
- Decreased Exercise Tolerance
CHRONIC COMPENSATED MR
If the patient is able to tolerated the acute MR phase (usually with medication), then the heart moves into a chronic compensated phase. The heart’s goal for this phase is to fix the pathology caused by acute MR:
- Improve Forward Cardiac Output
- Improve Pulmonary Congestion
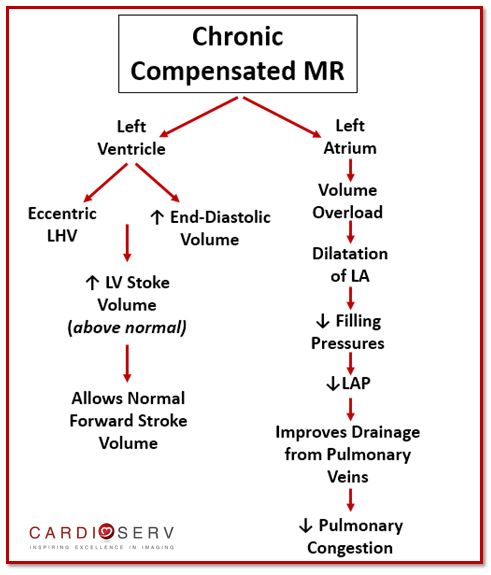
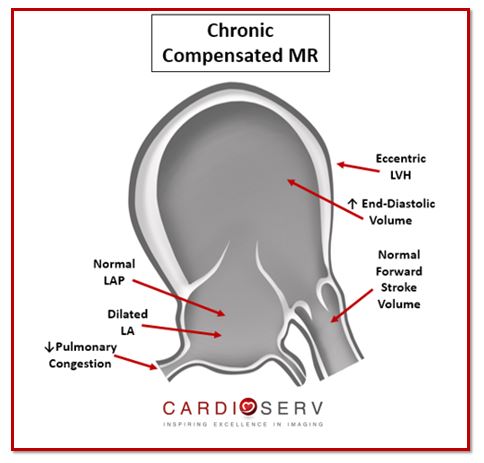
The left ventricle will develop eccentric LVH (read our past blog over this topic here) in order to deal with the larger stroke volume amount. With eccentric LVH, the ventricle increases in end-diastolic volume (increase in cavity size). This allows the LV stroke volume to increase above the normal range. This causes the forward stroke volume to rise from a low output level (from acute stage) to a normal output level.
In order for the left atrium to compensate for the regurgitant volume overload, it becomes enlarged. This allows the filling pressures to go from increased to a normal level. Which then improves the drainage of blood from pulmonary veins and relieves the pulmonary congestion.
Patients with chronic compensated MR will usually be:
- Asymptomatic
- Normal Exercise Tolerance
CHRONIC DECOMPENSATED MR
The last phase for a patient dealing with chronic MR, is when they enter chronic decompensated MR. It is unclear what causes a patient to transition from compensated to decompensated, and research is on-going. There are many theories as to what causes the heart to become decompensated, such as intolerance of LV to compensate for increase in regurgitant volume or due to calcium overload within cardiac myocyte.
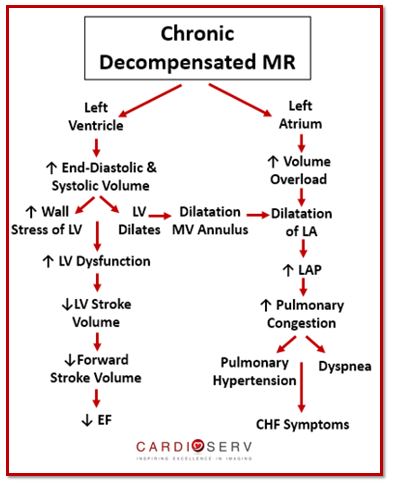
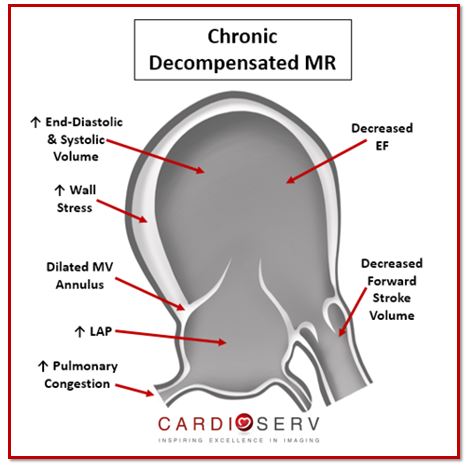
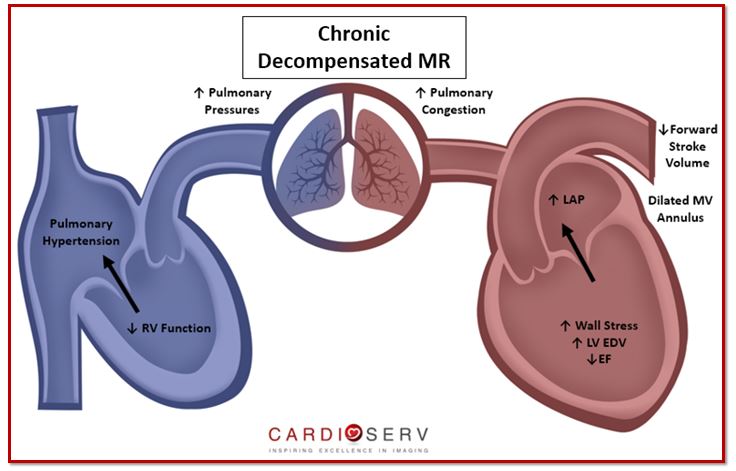
The hallmark sign for chronic decompensated MR is LV dysfunction. This happens when the LV continues to dilate and end-diastolic pressures increase. This puts a lot of stress on the chamber walls, which causes a decrease in LV stroke volume that leads to a decrease in forward SV (or cardiac output). This results in LV dysfunction and decreased ejection fraction (EF) because the ventricle cannot contract properly enough to compensate for the additional amount of regurgitant volume.
As the LV continues to dilate in cavity size, it causes the mitral annulus to expand as well. This causes the LA to continue to dilate and the severity of MR to increase. With the decreased cardiac output, more regurgitant volume is backing up within both ventricle and atrium. This causes the LAP to increase, which leads to an increase in pulmonary congestion. When this occurs, the patient will develop symptoms that mimic congestive heart failure (CHF), pulmonary hypertension and eventually right heart failure.
Patients with chronic decompensated MR will usually have:
- Symptomatic CHF
- Pulmonary Hypertension
- Right Heart Failure
- Low Exercise Tolerance
SUMMARY
In the last few weeks we have reviewed MV anatomy and explained primary/organic from secondary/functional MR. This week we helped explain how to further classify between acute, chronic compensated and chronic decompensated MR. This process plays a major role when diagnosing pathology identified on echo! It is also crucial that we report the mechanism of MR as well as acute versus chronic.
Keep an eye out for next weeks blog as we continue on the topic of MR mechanisms! The ASE elaborates on proper evaluation methods for common pathologies seen for both primary and secondary MR—and we at CardioServ want to easily break down these guidelines for you! We look forward to hearing feedback and comments from our readers!

Andrea Fields MHA, RDCS
Stay Connected: LinkedIn, Facebook, Twitter, Instagram
References:
Gaasch, W. H., MD, & Meyer, T. E., MD, PhD. (2008). Left Ventricular Response to Mitral Regurgitation. Circulation,118, 2298-2303. Retrieved June 29, 2017, from http://circ.ahajournals.org/content/circulationaha/118/22/2298.full.pdf
Zeng, X., Tan, T. C., Dudzinski, D. M., & Hung, J. (2014). Echocardiography of Mitral Valve. Progress in Cardiovascular Diseases , 55-73. Retrieved June 29, 2017.
Zoghbi, W. A., MD, Adams, D., RCS, RDCS, FASE, & Bonow, R. O., MD. (2017). Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation. JASE,30(4), 318-334. Retrieved June 6, 2017.
Zamorano, J. L., MD, & Badano, L. P. (2011). EAE/ASE Recommendations for the Use of Echocardiography in New Transcather Interventions for Valvular Heart Disease. JASE,24(9), 957-960. Retrieved June 6, 2017.