Over the past weeks, we have gone back to the basics to have a good understanding of what occurs during diastole in order to properly evaluate diastolic function. If you’ve missed our prior blogs, you can find them here:
Our goal by the end of this blog, is to have a clear understanding of what happens when the physiology of diastole becomes abnormal.
LET’S REVIEW WHAT WE KNOW!
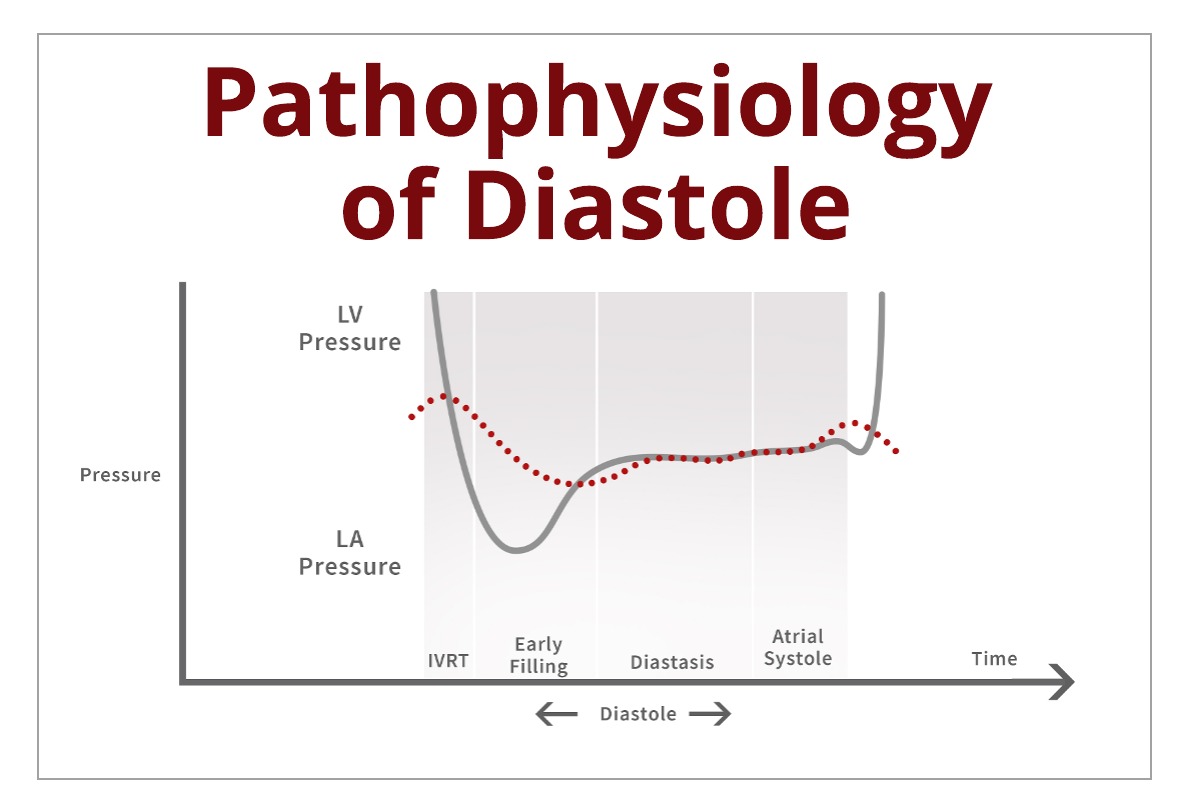
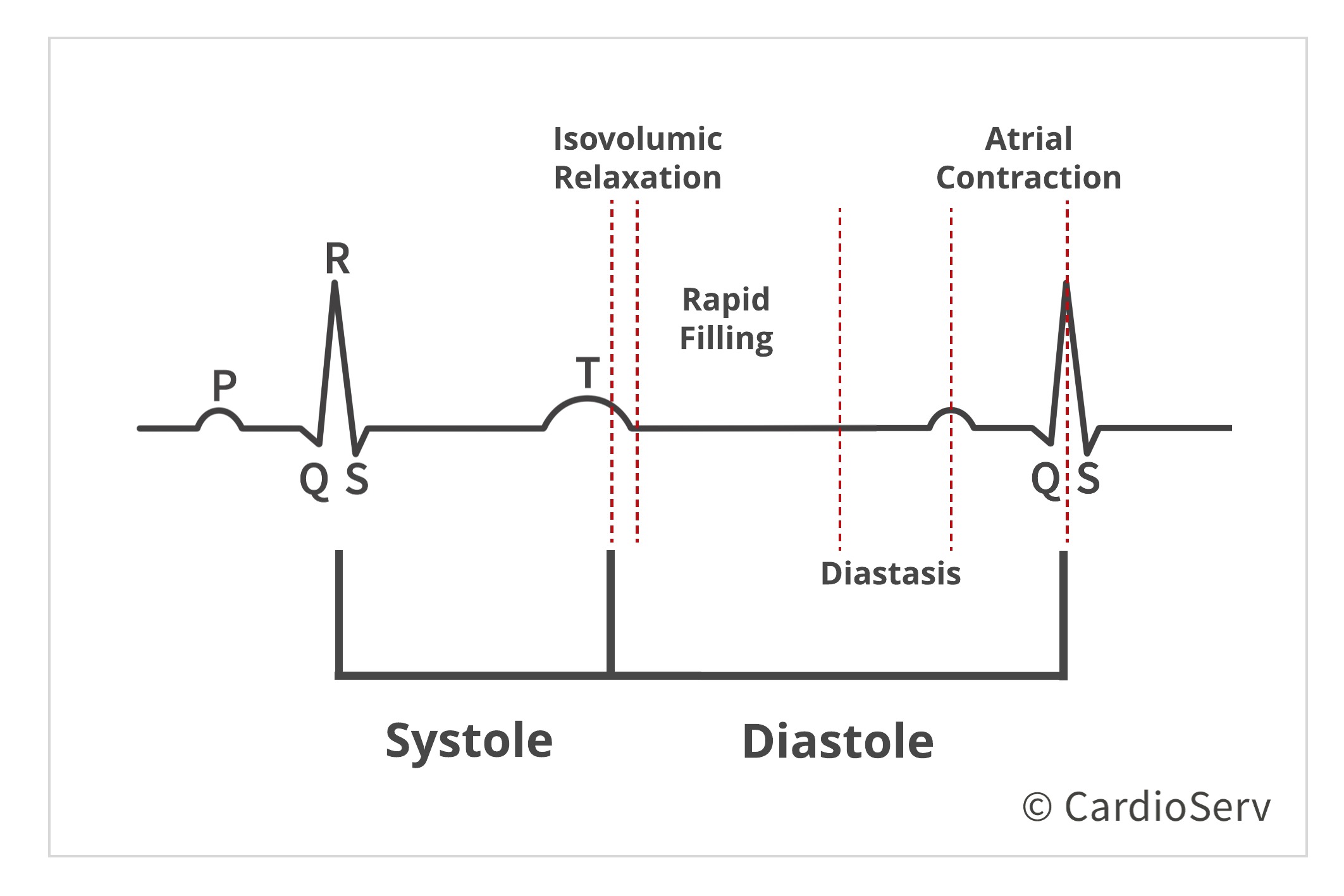
Evaluating diastole is based upon 4 stages:
- Isovolumic relaxation
- Rapid filling
- Diastasis
- Atrial Contraction
When we look at the four stages as a whole, we are evaluating the correct process in terms of:
- Diastolic Function
- Relaxation
- Filling Pressures
- Filling Properties
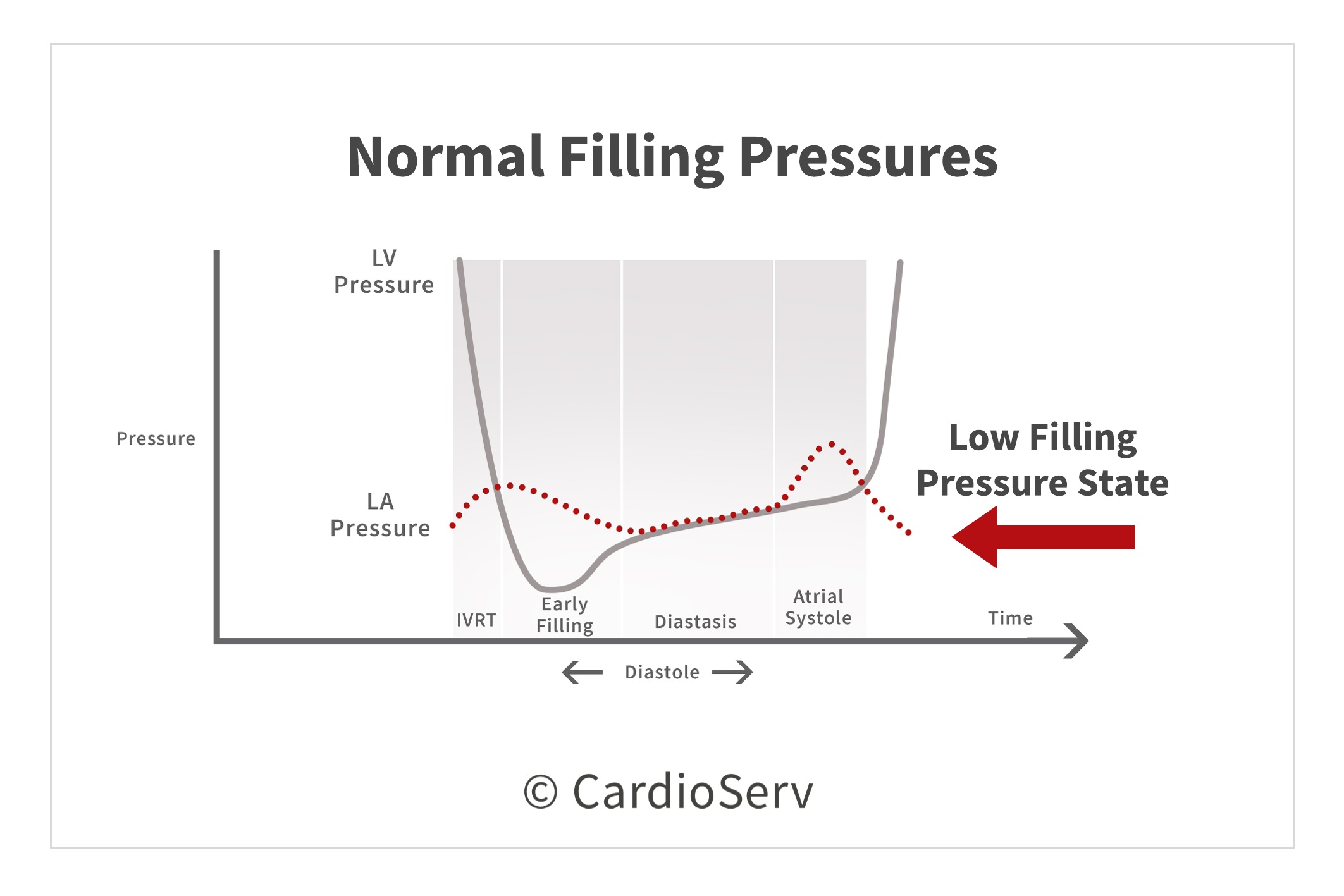
WHAT IS THE GOAL OF DIASTOLE?
The heart’s goal during diastole is to push blood from the left atrium, towards the apex of the left ventricle and fill an adequate amount of volume at a low pressure state. This occurs in a very rapid increment of time, 3-4x’s faster than the time to eject (systole).
 WHAT IS DIASTOLIC DYSFUNCTION?
WHAT IS DIASTOLIC DYSFUNCTION?
If any stage or process of diastole falls out of the normal scope, pathophysiology is present. Patho– meaning pathology and physiology– meaning the normal process of how diastole occurs. Therefore when the heart is unable to properly fill at a low pressure state, diastolic dysfunction is present.
WHAT HAPPENS WITH DIASTOLIC DYSFUNCTION?
The main consequence of diastolic dysfunction is due to elevated filling pressures. Let’s break this process down:
- The ventricle cannot relax sufficiently or in enough time to allow proper filling at a low pressure state
- This tells us the ventricle has abnormal relaxation and increased stiffness
- Filling pressures increase (including left atrial pressure) to maintain adequate amount of end-diastolic volume
- Increased pressures occur in order for the ventricle to efficiently pump out the proper amount (cardiac output) necessary for the body
When the heart increases the filling pressures, it is adding a ample amount of stress and additional workload. As time goes on, the diastolic dysfunction worsens. The heart continues to increase in stiffness with decrease compliance. As filling pressures rise, pulmonary congestion begins to build up causing symptoms of dyspnea and decreased exercise tolerance.
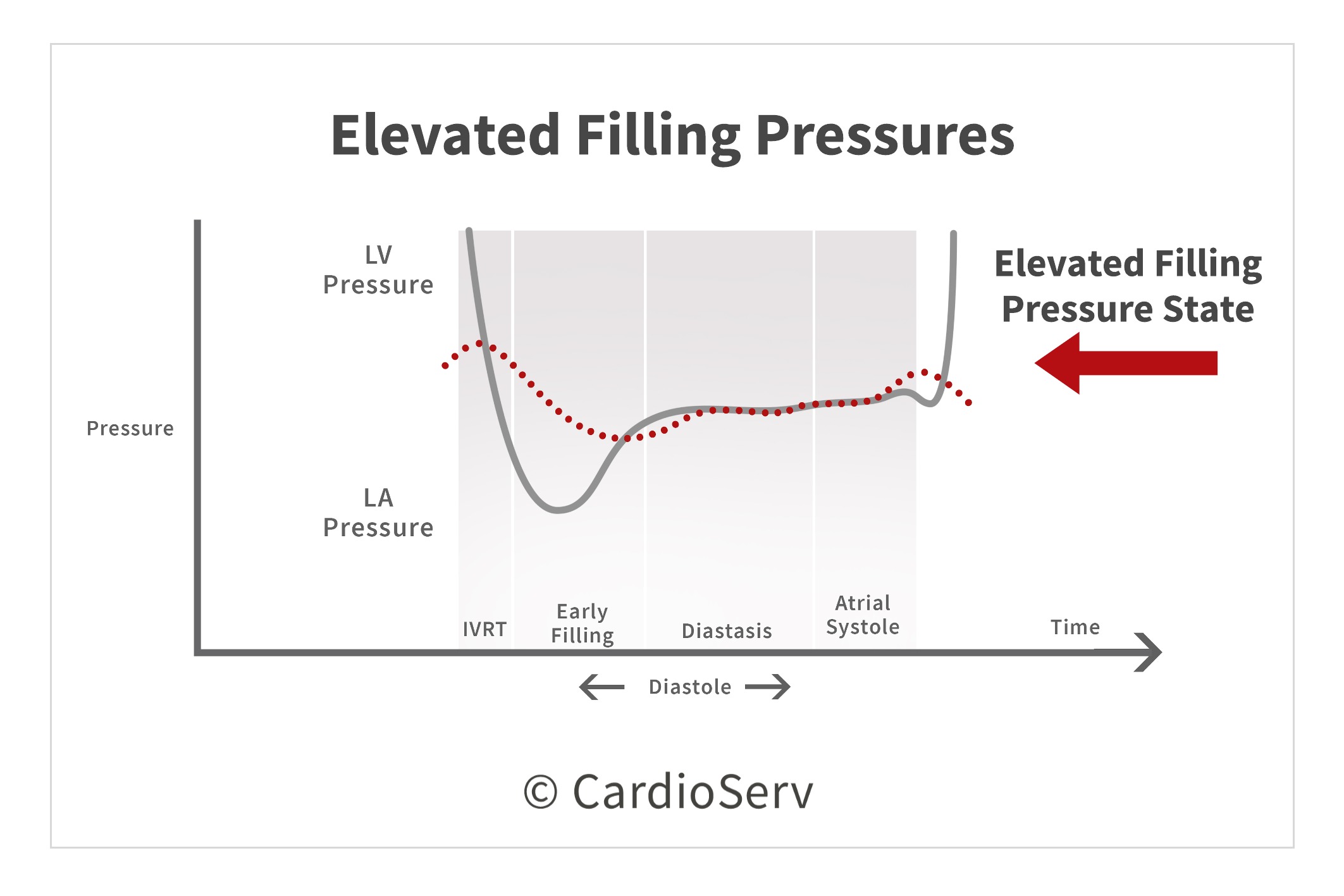
As advanced stages occur with higher filling pressures, the heart cannot keep up the extra workload and chambers change in geometry. Both the atrium and ventricle will become enlarged to accommodate the high pressures and volume. The heart eventually goes into heart failure, with a decreased exercise tolerance.
HALLMARK SIGNS OF DIASTOLIC DYSFUNCTION:
Hallmark signs of LV diastolic dysfunction include:
- Impaired relaxation
- Loss of restoring forces (inability of energy to be stored during systole)
- Reduced diastolic compliance (increased stiffness)
- Elevated filling pressures
COMMON CAUSES OF DIASTOLIC DYSFUNCTION:
As research continues, it is assumed that diastolic dysfunction is the primary cause of heart failure with preserved LV ejection fraction (HRpEF). There are many symptoms that can present with heart failure with dyspnea presenting in the majority of patients. Dyspnea can also be caused by many other cardiac and non-cardiac diseases. It is vital we rule out other possibilities causing dyspnea before jumping to conclusions and claiming diastolic dysfunction as the main source.
Diastolic dysfunction can also be the secondary result of many cardiac abnormalities:
- Heart failure
- Dyssynchrony
- Constriction
- Cardiomyopathies
- Valvular disease
- Ischemia
OUR ROLE IN EVALUATING FOR DIASTOLIC DYSFUNCTION:
The main reasons for a patient to be screened for diastolic dysfunction are:
- Symptoms/signs of heart failure in patients with preserved LV ejection fraction
- Estimation of LV filling pressures with known cardiac disease
- Assessment of cardiovascular risk
It is our job as sonographers and physicians to understand the physiology of diastolic function in order to properly evaluate our patients for diastolic dysfunction. This involves a full examination to help determine the cause of the pathophysiology being suggested on our studies. It’s vital we understand each patient is different from the next and a thorough evaluation is necessary.
SUMMARY
Diastolic dysfunction is an independent predictor of all-cause mortality. As the diastolic dysfunction stages advance, the filling pressures will continue to increase causing worse outcomes. Diastolic dysfunction can present for several years before being clinically evident. There are many cardiac abnormalities that can cause dysfunction. This is why evaluation is a vital part our of routine examinations for every single patient we encounter.

Andrea Fields MHA, RDCS
Stay Connected: LinkedIn, Facebook, Twitter, Instagram
References:
Gillebert, T. C., Pauw, M. D., & Timmermans, F. (2013). Echo-Doppler Assessment of Diastole: Flow, Function and Hemodynamics. Education in Heart, 99, 55-64. Retrieved November 20, 2017, from https://pdfs.semanticscholar.org/deda/8ed40076f7bbb1da2668d190d15af9947c2d.pdf.
Nagueh, S. F., MD, Smiseth, O. A., MD, & Appleton, C. P., MD. (2016). Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and European Association of Cardiovascular Imaging. American Society of Echocardiography, 29(4), 277-314. Retrieved October 31, 2017, from http://asecho.org/wordpress/wp-content/uploads/2016/03/2016_LVDiastolicFunction.pdf
Andersen, O. S., MD, Smiseth, O. A., MD, & Dokanish, H., MD. (2017). Estimating Left Ventricular Filling Pressures by Echocardiography. Journal of the American College of Cardiology,69(15), 1937-1948. Retrieved November 29, 2017.
Mitter, S. S., MD, Shah, S. J., MD, & Thomas, J. D., MD. (2017). A Test in Content: E/A and E/e’ to Assess Diastolic Dysfunction and LV Filling Pressures. Journal of the American College of Cardiology,69(11), 1451-1464. Retrieved November 29, 2017.