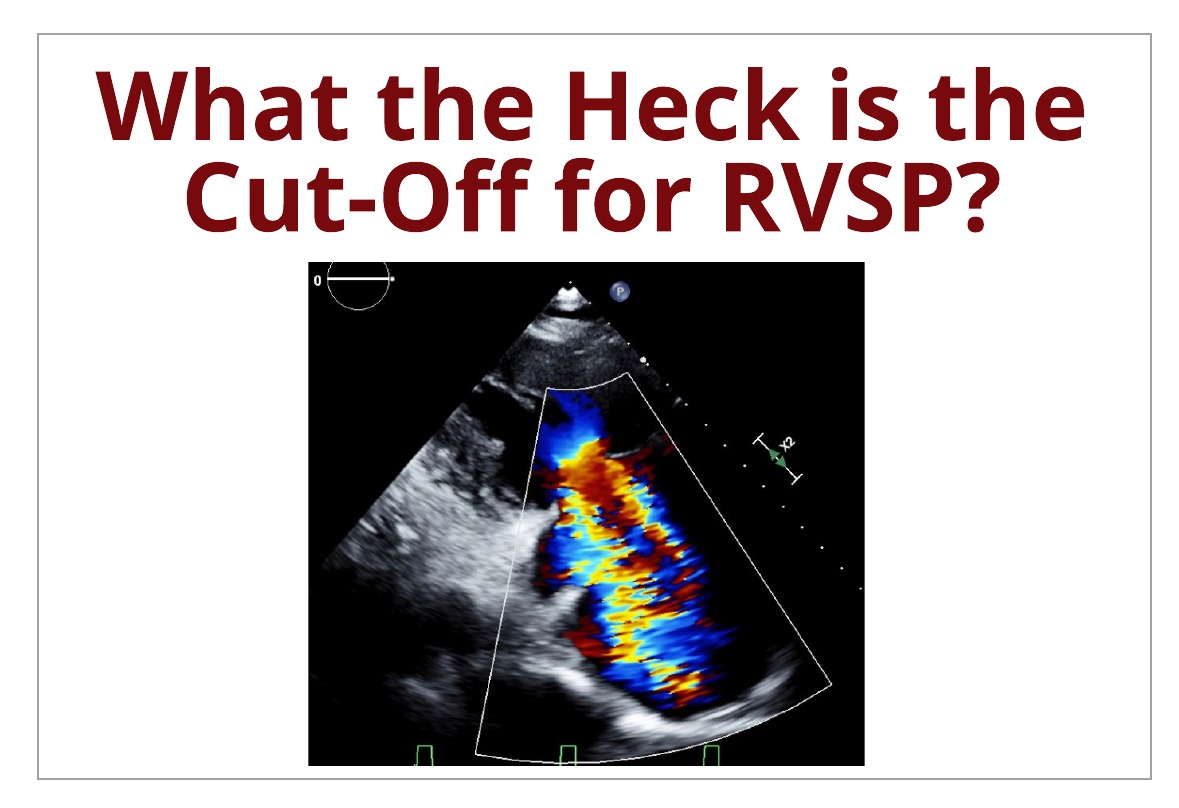
Us clinicians commonly ask the same popular question in our field, “What is the cut-off ranges for pulmonary hypertension?!” We want to help better understand the basics of determining the presence of pulmonary hypertension with echocardiography.
First let’s start with one important key item to understand: Cardiac catheterization is the gold standard to obtaining pulmonary artery pressures for evaluating the severity of pulmonary hypertension. That’s all we need to know, the end.
KIDDING! It’s obvious we cannot send every patient to get an invasive procedure done in order to rule out pulmonary hypertension (PH). That is why we rely on echocardiography to help give us an insight, non-invasively, on the right heart pressures.
- Cath calculates the mean pulmonary artery pressure (mPAP) and systolic pulmonary artery pressure (sPAP).
- Echo calculates the right ventricular systolic pressure (RVSP).
The definition of PH is a pathophysiological condition determined when there is an increase of the MEAN pulmonary artery pressure is > 25 mmHg at rest, obtained by invasive right heart catheterization.
Unfortunately non-invasive echo obtained values got left out of the definition. It’s important to understand these values are not the same measured items …. WE CANNOT COMPARE VALUES OF CATH MPAP TO ECHO RVSP! But let’s talk about what we can do with echo…
RVSP
RVSP obtained via echo can provide insight & good correlation to the invasively obtained systolic pulmonary artery pressure (sPAP). **NOTE: They are not the same measured values still & we are talking about sPAP (not mPAP).**
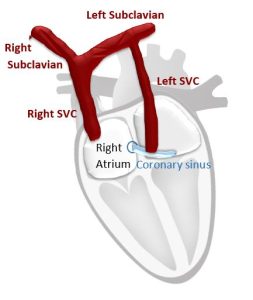
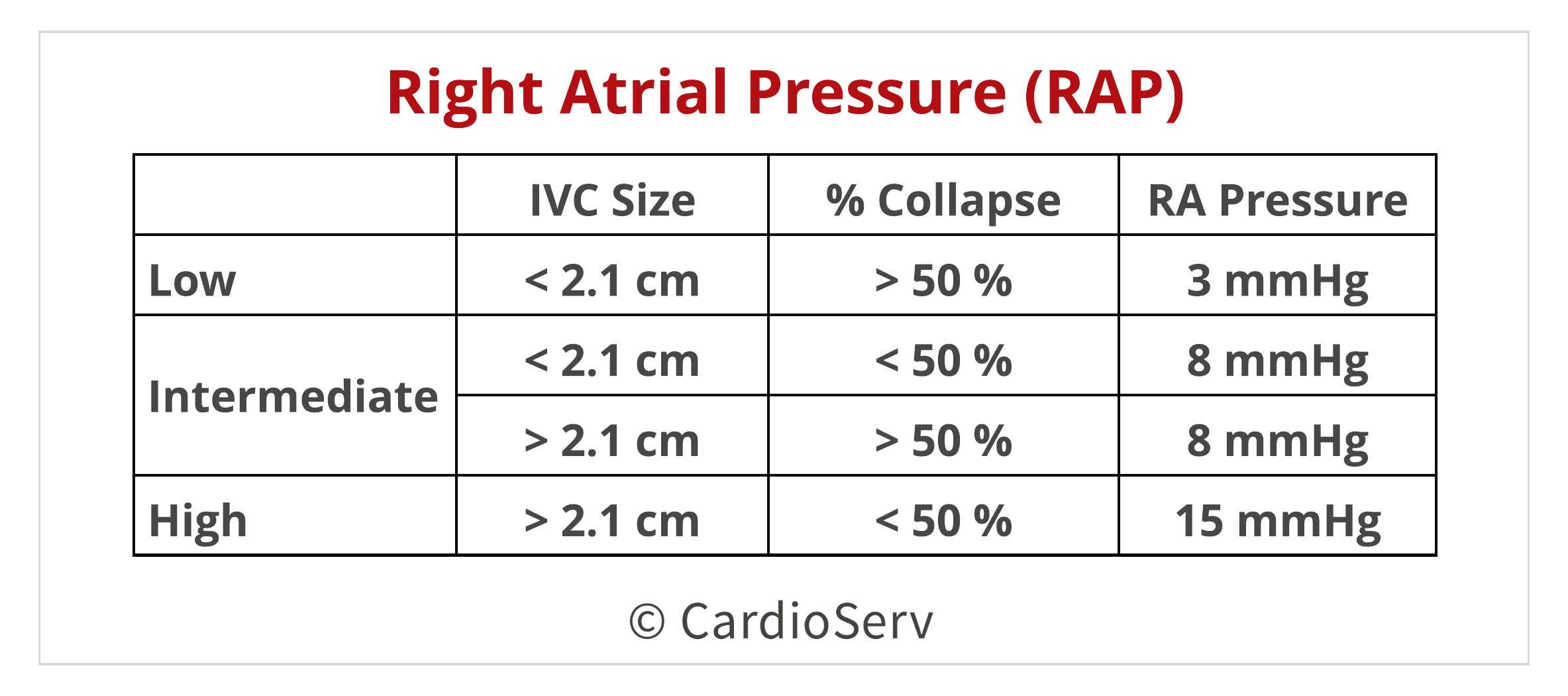
To calculate the RVSP, we use the simplified Bernoulli equation (4V²) and add the estimated right atrial pressure (RAP).
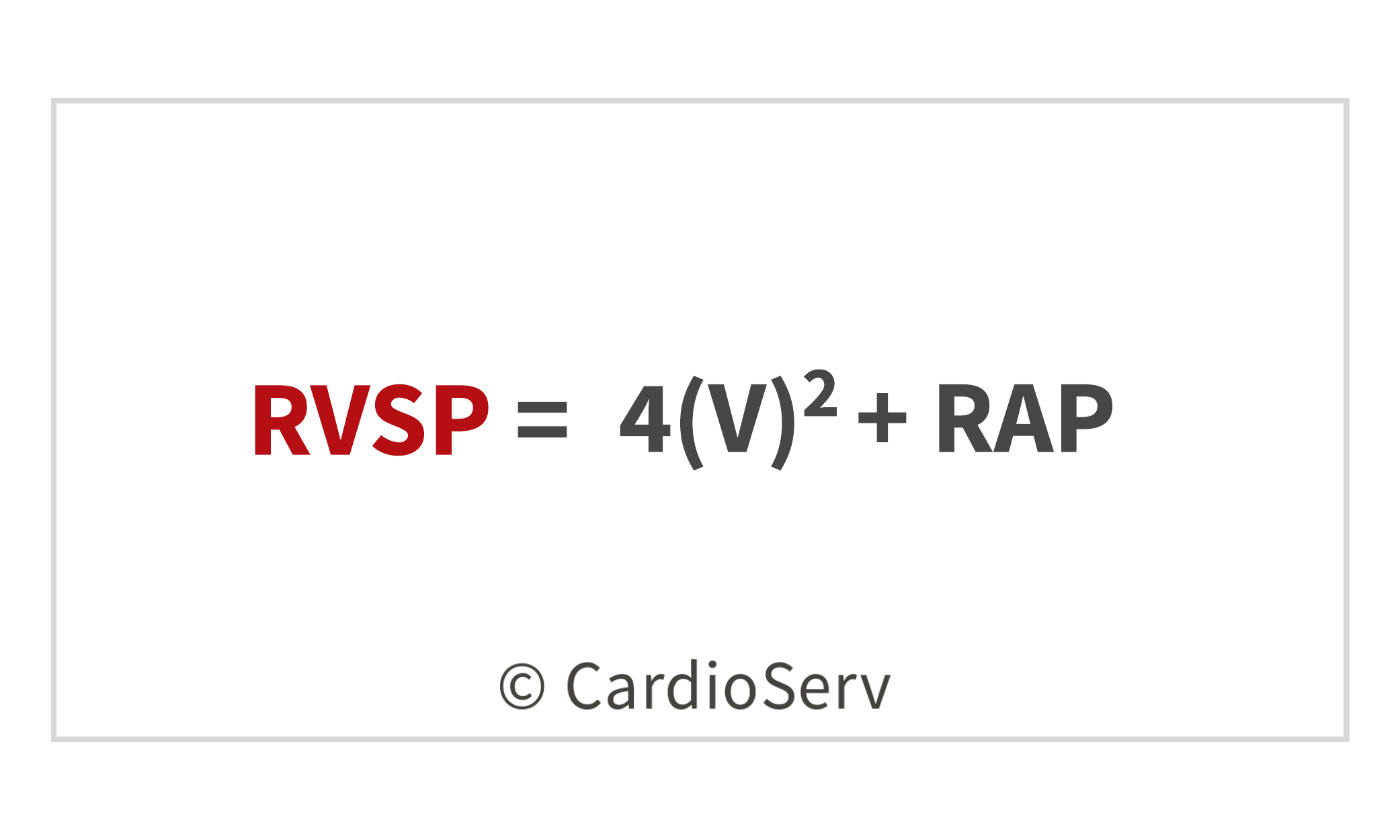
Simplified Bernoulli equation allows us to take echo obtained Doppler velocities and convert them to pressures. We do this by measuring the peak tricuspid regurgitation jet, which represents the pressure difference between the right atrium and ventricle. The second part of the equation (RAP) is determined by assess the size and collapsibility index of the IVC to determine the recommended RAP specific value [3 , 8, 15 mmHg].
RVSP LIMITATIONS
Of course, there are always limitations to everything non-invasive. RVSP has limiting factors:
- Dependent upon increased age and body mass index (BMI)
- Flow dependent on certain variables
RVSP CUT-OFF VALUE
Let’s talk about the good stuff …. cut-off values. According to the latest ASE guideline paper on Echocardiographic Assessment of Right Heart in Adults (2010), the following indicate elevated right ventricle systolic and pulmonary artery pressures: (*in the absence of RVOT obstruction or pulmonary stenosis)
- Tricuspid Regurgitation Velocity > 2.8- 2.9 m/s
- Assigned RAP of 3 mmHg
- Will correspond to invasive elevated sPAP of approximately 36mmHg
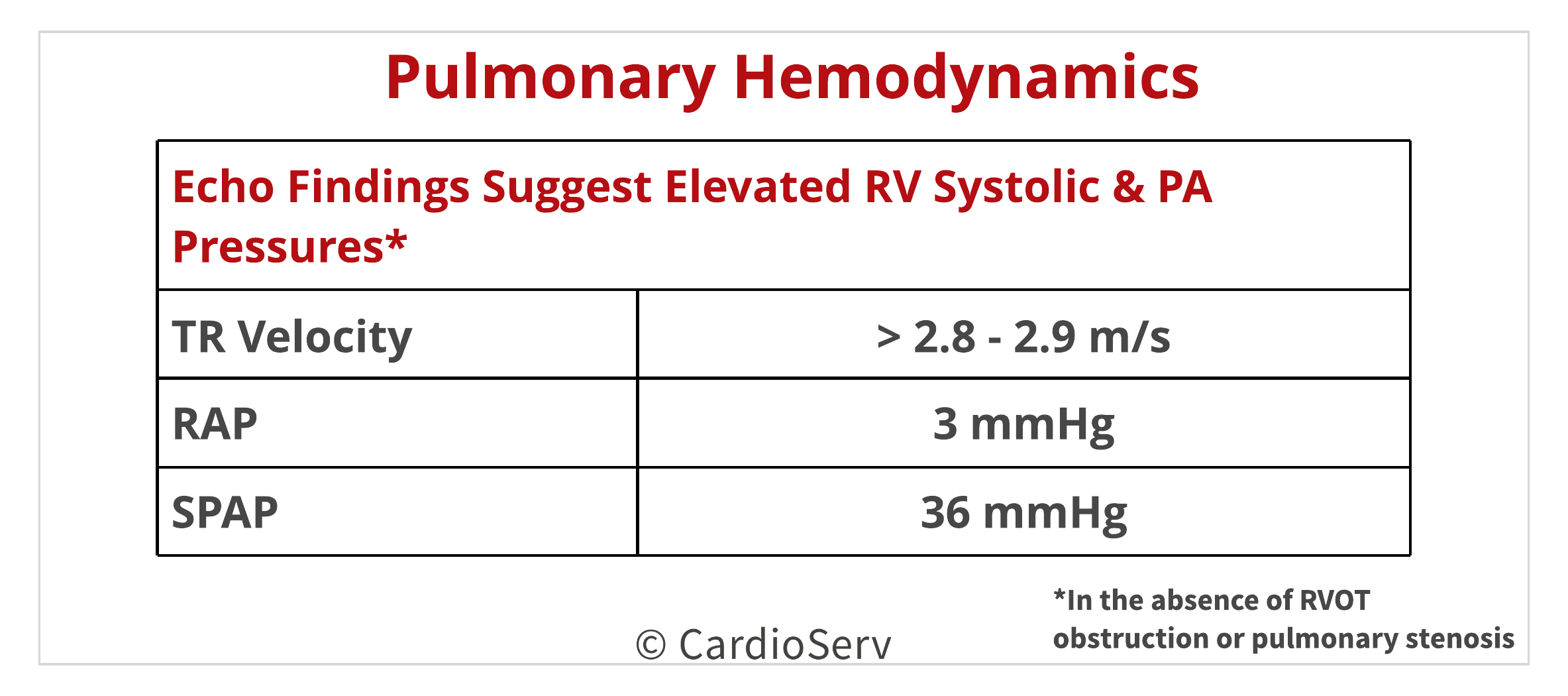
- RVSP 34.2 – 36.6 mmHg corresponds sPAP 36 mmHg
- Normal reference range of invasive sPAP: 15-30 mmHg
But remember the true definition of PH? Let’s re-look at it… “a pathophysiological condition determined when there is an increase of the MEAN pulmonary artery pressure is > 25 mmHg at rest, obtained by invasive right heart catheterization.”
…. but the definition does not include sPAP, which is the value that correlates with non-invasive RVSP? Here is where the confusion arises when determining the reference ranges for PH using echo.
- ACC/AHA expert consensus document for PH recommends further evaluation in those experiencing dyspnea with estimated RVSP > 40 mmHg.
- ASE recommends evaluation to determine the present of PH if the RVSP > 35-40 mmHg and other clinical symptoms correlate.
Notice the difference in cut-off ranges for PH between the 2 organizations? Here is why an agreement cannot be made:
- ASE recommends using RAP specific values [ 3, 8, 15 mmHg] and not value ranges [ 5-10 , 10-15, 15-20 mmHg].
- As clinicians, we have not consistently (across the WORLD) shifted from RAPs of ranges to specific values yet.
- This causes a gap range of 5 mmHg that alters the cut-off value from being either > 35 mmHg or > 40 mmHg.
Therefore a recommended cut-off value is indeterminate because of the variability in assigning RAP. Let me give an example of the SAME patient, just assigning different RAP values ….
Example #1:
- TR Velocity: 2.8 m/s
- RAP: 3 mmHg (specific value)
- RVSP: 34 mmHg
Example #2:
- TR Velocity: 2.8 m/s
- RAP: 10 mmHg (range values)
- RVSP: 41 mmHg
The outcome of assigning specific vs. range RAP places the SAME patient into either normal and abnormal cut-off ranges.
- RAP of 3 mmHg with RVSP 34 mmHg = ASE & AHA/ACC suggest the patients does NOT have elevated pressures
- RAP of 10 mmHg with RVSP 41 mmHg = ASE & AHA/ACC suggest the patient DOES have elevated pressures
We need to avoid having the same patient be diagnosed with PH, then 1 year follow up be told they do not have PH due to variability in assigning RAP.
CONCLUSION
- We need to make the recommended shift to assigning RAP of specific values [ 3 , 8 , 15 mmHg].
- Determine the RAP after full evaluation of IVC and the collapsibility index. (No more assigning RAP at the beginning of the study!)
- Factor in patient clinical symptoms into determining presence/absences elevated pressures.
- Use a caution reference range of 35-40 mmHg as extra cushioning for variability of RAP assigning.
- RAP specific values = > 35 mmHg suggestive of elevated pressures
- RAP range values = > 40 mmHg suggestive of elevated pressures
WANT TO READ MORE ON THIS TOPIC AND EARN CAT. 1 AMA CMES? CLICK THE LINK BELOW!


Andrea Fields MHA, RDCS