Last Updated on January 30, 2024 by Hannes van der Merwe
We recently posted a 2-part blog series on how to calculate LV Mass (LVM) and one of our readers provided some great feedback regarding the impact of height on LVM. We thought this reader’s comment was worth sharing and answering.
Reader: Using body surface area to normalize LVM will misclassify obese hypertensive patients and artificially increase the proportion of concentric LV remodeling. As also recommended by EACVI/ASE (Marwick TH et al. J Am Soc Echocardiogr 2015;28:727-54.), using height raised to validated powers (called allometric signals) might be much more appropriate to identify obesity-associated LVH. The most used allometric exponent is 2.7. Normalization of LVM for height in meters raised to the power of 2.7 near doubles the population attributable risk of LVH.
Thank you for sharing this information with our readers. We also found that article useful in explaining how height factors into LVM. The article explains how LVM and volumes bear an approximately quadratic relationship with height in men rather than approximately cubic relationship with height in women. The paper went on to explain the effects of gender on LVM which indicates that after adjustment for blood pressure and anthropometric parameters, LV volume and LVM are higher in men than in women. These differences persist when values of LVM are corrected for fat-free mass. This sex difference may explain the surprising lack of consensus in appropriate indexation of LVM, as it impacts the optimal method for indexing LVM for body height.
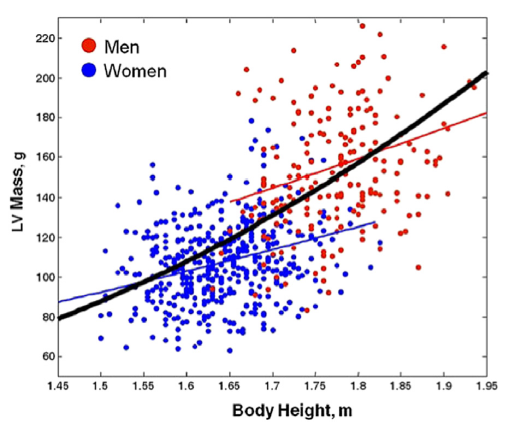
LVM CALCULATED BY THE DEVEREUX FORMULA IN MEN AND WOMEN BY HEIGHT
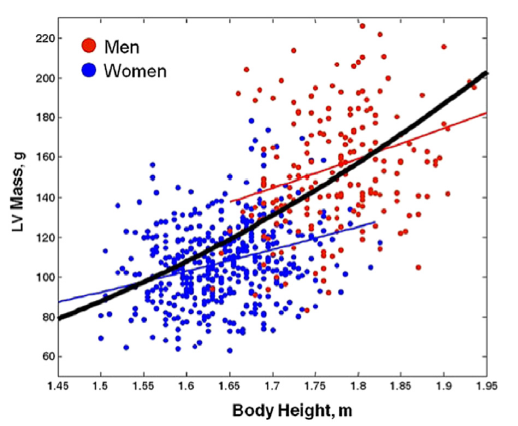
The graph displays LVM, calculated by the Devereux formula (unidimensional 2D measurements) in healthy patients.
- The red line represents the body height–LVM relationship in men.
- The blue line represents the body height–LVM relationship in women.
- The black line represents the exaggeration of nonlinearity in the height–LVM relationship when the confounding effect of sex is neglected.
- Using the allometric index 1.7, the body height– LVM relationship in men (red) and women (blue) is parallel and indexation for body height is optimally achieved by height (ht) 1.7 in both sexes.
- However, when an allometric exponent is computed for males and females considered together (thick black line) without adjustment for gender, there is an exaggeration of nonlinearity in the height–LVM relationship (allometric index 2.7).
- This has important clinical and epidemiological implications, resulting in marked overestimation of the prevalence of LV hypertrophy in short subjects and a marked underestimation in tall subjects. The appropriate indexation remains an issue of contention.
ASE COMMENTS
In the ASE 2015 Chamber Quantification Guidelines they acknowledged that whether to use height, weight, or BSA as the indexing term remains controversial.
- Studies suggest that indexing to height raised to allometric powers such as 1.7, 2.13, and 2.7 has advantages over indexing to BSA, especially when attempting to predict events in obese patients.
- However most large population studies reporting LV mass have indexed to BSA.
- Calculation of relative wall thickness (RWT) with the formula (2 x PWd)/(LVIDd) permits categorization of an increase in LV mass as either:
- Concentric hypertrophy (RWT > 0.42)
- Eccentric hypertrophy (RWT < 0.42)
- Identification of concentric remodeling (normal LV mass with increased RWT)
ASE RECOMMENDATIONS
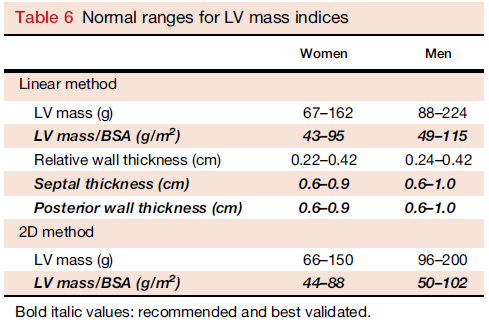
The final recommendations from the ASE for LVM states that in normally shaped left ventricle, both M-mode and 2D echocardiographic formulas to calculate LV mass can be used. Normal values for these techniques should be reported indexed to BSA.
- Reference upper limits of normal LV mass by linear measurements are 95 g/m2 in women and 115 g/m2 in men.
- Reference upper limits of normal LV mass by 2D measurements are 88 g/m2 in women and 102 g/m2 in men with 2D methods.
- Because 3DE is the only echocardiographic technique that measures myocardial volume directly, without geometric assumptions regarding LV shape and distribution of wall thickening, this technique is promising and may be used in abnormally shaped ventricles or in patients with asymmetric or localized hypertrophy.
- Limited upper normal limits of 3D echocardiographic LV mass data are currently available in the literature but are insufficient to substantiate recommendations for reference values
TAKE-AWAY
Be aware that there is a relationship of height that is not corrected by indexing by BSA which may result in the overestimation of the prevalence of LV hypertrophy in short subjects and a marked underestimation in tall subjects. ASE recognizes that indexing to height raised to allometric powers such as 1.7, 2.13, and 2.7 has advantages over indexing to BSA, especially when attempting to predict events in obese patients, however most large population studies reporting LV mass have indexed to BSA. ASE current recommendations, due to the large database of LVM reporting, currently is to index to BSA.
We love it when our readers provide feedback and education for our readers, so please keep your comments coming!

Judith Buckland, President
References
- Marwick, T. H., PhD, Gillebert, T. C., MD, & G. A., MD. (2015). Recommendations on the Use of Echocardiography in Adult Hypertension. JASE,28(7), 1-12. Retrieved March 1, 2017, from http://asecho.org/wordpress/wp-content/uploads/2015/07/2015_Hypertension.pdf
- Lang, R. M., MD, Badano, L. P., MD, & Mor-Avi, V., PhD. (2015). Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. JASE, 28(1), 1-53. Retrieved March 1, 2017, from http://asecho.org/wordpress/wp-content/uploads/2015/01/ChamberQuantification2015.pdf