We love to hear from our readers and have them share interesting case studies with us. This week Patrice McKay, will share her story of an interesting find while in the ER. Patrice is featured in this week’s sonographer spotlight. Please check it out and learn about her inspiring journey into cardiac ultrasound and her recent volunteer work. Take it away Patrice…
I got called to the emergency room for a STAT echo. I was informed it was a suspected STEMI patient but upon evaluation by the cardiologist for intervention, he was not convinced. He ordered an echo and informed me he was looking for a LV outflow obstruction.
As I made my way through the study and put color on the apical views, I immediately noticed turbulence in the LVOT and left atrium with moderate eccentric Mitral regurgitation.
I started to think the patient had an LVOT obstruction, just like the ER physician mentioned he was looking to find. Upon further assessment, the patient had SAM (systolic anterior motion) of the mitral valve. The extreme anterior motion of the mitral valve into the LVOT was causing the LVOT turbulence and eccentric MR.
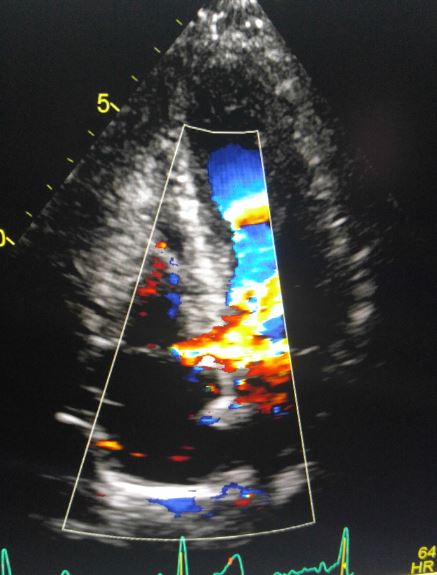
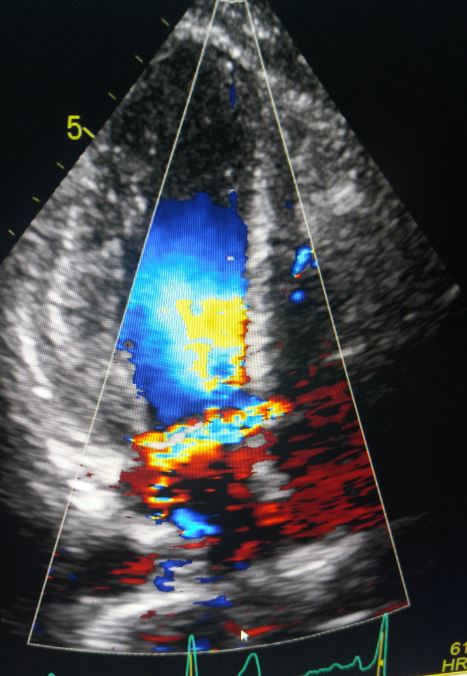
As I continued to scan, I also noticed flow crossing the basal interventricular septum. Upon further scrutiny I noticed a defect in the peri-membranous septum. I informed the cardiologist and waited to read the final report to confirm my findings.
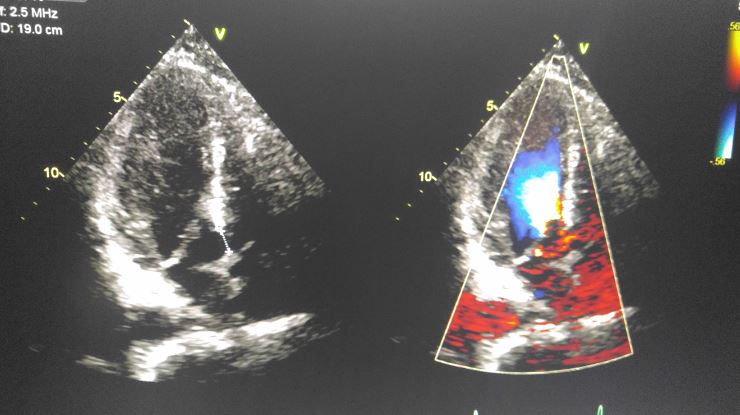
The cardiologist reported flow from the left ventricle to the right atrium! Had I missed that? I went back and reviewed my images and sure enough there was flow in the right atrium from the left ventricle. I had not noticed that while scanning due to all the turbulence and difficulty of the image window, but the cardiologist had picked it up.
I suddenly remembered an article I had seen on my social media feed about a defect between the LV and RA called Gerbode’s defect. Intrigued, I wanted to learn more about it. My pediatric echo reference book did not mention it. I thought, “how new is this anomaly?” As it turns out this defect has been documented since 1857! I decided to research the topic and share my findings so that I could help other sonographers.
Documented Gerbode’s defect dates back to 1857. The defect was named after Dr. Frank Gerbode in 1958 after he successfully closed ventricular-to-right atrial shunts on a series of 5 patients.
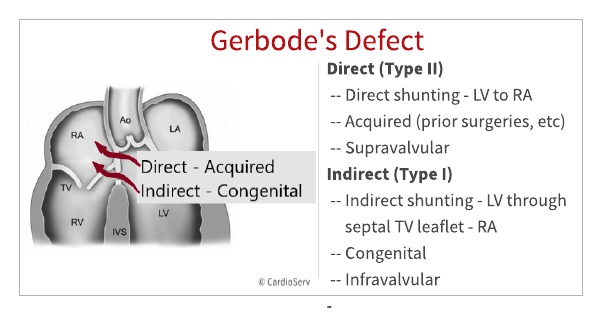
Gerbode’s defect is defined as abnormal shunting between the left ventricle and the right atrium resulting from either a congenital defect or prior cardiac insults. Gerbode’s seems to be mostly congenital however there have been reports of an increase in the acquired type as a result of bacterial endocarditis.
Gerbode’s Defect is classified as either direct or indirect, based on the route of the shunt.
While transthoracic echo is sensitive for detecting shunts, TEE is the better choice to distinguish whether the communication is directly from the LV to RA via the septal leaflet of Tricuspid valve.
Gerbode’s defect is a ventriculo-atrial communication occurring between the left ventricle and right atrium through the membranous portion of the ventricular septum. It is classified in 2 ways depending on the route of the shunt flow.
Being aware of this defect helps us to pay closer attention to turbulent or eccentric jets in the right atrium. Jets that we often attribute to significant TR or just bleeding of color on the image.
Thank you Patrice for this great article. We appreciate you sharing this case with us. When identifying Gerbode’s Defect it is necessary to accurately determine the location of the shunt communication. Unfortunately, this is often difficult to do. In the upcoming weeks, we will share tips and pitfalls to avoid when imaging Gerbode’s Defect with echocardiography.

Patrice McKay, RDCS – Guest Writer
Connect with Patrice on LinkedIn
References




Sep
2019
Sep
2019
Sep
2019